Did you know that your brain contains over 100 billion cells? About half of those cells are neurons1, specialized brain cells that communicate by sending electrical and chemical signals to each other and other organs and tissues to produce thoughts, emotions, and actions. When the brain is healthy, neurons communicate by sending signals one at a time or in small groups to regulate normal thinking and behavior. If something goes wrong in these signaling processes, thousands of neurons can start to send signals all at the same time.
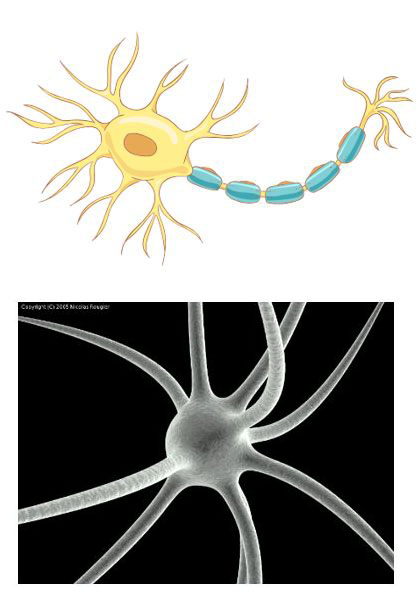
Figure 1.
A drawing of a neuron (left) and a neuron as seen under the electron microscope (right).
[Source: https://bioart.niaid.nih.gov/bioart/197; https://commons.wikimedia.org/wiki/File:Neuron-SEM.png]
Too much brain activity all at once is known as a seizure2. During a seizure, increased electrical activity in the neurons can cause a variety of symptoms including involuntary movements, loss of awareness, loss of consciousness, and even death in severe cases. Anything that disrupts the normal functioning of neurons, such as illness, brain damage, or a developmental disability3, has the potential to cause a seizure. Up to 10% of people will experience a seizure at some point in their lives.
A single seizure does not necessarily indicate long-term brain disease. However, seizures are a feature of epilepsy4, a chronic brain disorder characterized by at least two unprovoked seizures. Epilepsy is one of the oldest documented diseases. One of the first records of the disease comes from ancient Mesopotamian tablets written 4,000 years ago. The exact causes of epilepsy are unknown. There are genetic and environmental factors involved, and epilepsy can be acquired during life after illness or injury to the brain. In cases of acquired epilepsy, the condition may not develop until years or decades after the initial event that caused it.
Multiple treatments are available for people with epilepsy to reduce the severity and frequency of seizures. These medications typically need to be taken long-term to control seizures, and some people may need to take them for the rest of their lives. Unfortunately, these treatments don’t work for everyone. About one third of people with epilepsy do not respond to any available treatments. In these cases, patients may need to undergo surgery to remove the area of the brain causing seizures. To date, there are no treatments that can be taken for a short time to modify the altered brain activity in people with epilepsy to prevent seizures after the treatment is stopped.
Dr. Avtar Roopra is a neuroscientist whose research focuses on understanding what causes epilepsy to help develop better treatments. Previous research by Dr. Roopra and colleagues at institutions around the world identified the gene Enhancer of Zeste Homolog 2 (EZH2) as playing a role in the development of epilepsy. In mouse models5 of epilepsy, mice without EZH2 had more frequent and more severe seizures compared to controls. “EZH2 acts like a brake on the brain, stalling the development of seizures and seizure disorders,” commented Dr. Roopra. Once this gene was identified, the next step was to understand how EZH2 protected the brain. “We thought if we could figure that out, we might be able to develop ways to boost the brain’s own defenses against damage from seizures,” explained Dr. Roopra.
As Dr. Roopra and colleagues began their research into EZH2, Olivia Hoffman joined Dr. Roopra’s laboratory as a PhD student. “My goal was to find out how EZH2 acted in the brain and how it was involved in epilepsy,” recalled Olivia, saying, “The easiest way to do that is to see what happens when you take it away.” In initial experiments, Olivia developed mouse models lacking the EZH2 gene and compared seizure outcomes in mice with the gene (controls) and without (experimental). She found the mice without the EZH2 gene had worse outcomes, with more severe and more frequent seizures.
Next, Dr. Roopra and Olivia analyzed the role of different genes in the neurons of the mouse models using RNA sequencing6. RNA sequencing is a technique that allows scientists to analyze genetic expression at the level of the cell. The researchers used RNA sequencing on specialized cells from a region of the brain called the hippocampus7. They chose these cells because, unlike many other cell types, they don’t die after a seizure. They found 10,556 genes that were expressed in neurons of both control and experimental mouse models. Nearly 60% of the genes had differences in expression between the mice with EZH2 and those without. In particular, the researchers noticed a group of genes whose expression increased after seizures in control mice and increased even more in mice without EZH2.
Dr. Roopra developed an algorithm that used mathematical instructions to sort through the data and identify the factors behind the changes in gene expression they observed, called Mining Algorithm for GenetIc Controllers (MAGIC). This algorithm identified the gene signal transducer and activator of transcription 3 (STAT3) as a primary factor driving the changes in gene expression after seizures. Follow-up experiments showed that STAT3 is more highly expressed in every cell type in the mouse brain after seizures, as well as in the brains of people with epilepsy.
STAT3 is known to play an important role in inflammation8, and several inflammatory diseases can be treated with a class of medications called Janus kinase (JAK) inhibitors that target the STAT3 protein. Olivia wanted to see whether treating mouse models of epilepsy with a JAK inhibitor might impact gene expression. She reviewed the scientific literature on JAK inhibitors and identified one that seemed the most likely to affect neurons, called tofacitinib. Her plan was to give the medication to mice just after they experienced seizures but before they developed epilepsy.
Dr. Roopra, Olivia’s supervisor, initially didn’t think these experiments were a great idea. “Other labs had tried this kind of experiment before, and it had been unsuccessful,” explained Dr. Roopra. “I didn’t think it was worth trying again.” Olivia insisted that this was the logical next step in her research. “The data clearly pointed to the role of STAT3 in epilepsy, and I was just following the data,” she added.
The first set of experiments with tofacitinib were unsuccessful. The mice who received tofacitinib went on to develop epilepsy just like the controls. Olivia didn’t give up. A colleague had mentioned that treatment once epilepsy had started could help improve cognitive function, even if seizures continued. Olivia tried the same tofacitinib experiment again, this time giving the treatment after the mice had already developed epilepsy. The researchers didn’t know what to expect from the experiment, but they were thrilled by the result. “After 10 days of this treatment, the seizures just completely went away in 80% of the experimental mice,” recalled Olivia.
To understand what was happening in the mouse brains, Olivia took samples of tissue from the hippocampus of mice without epilepsy, control mice after 2 months of treatment, and experimental mice after 2 months of treatment. She used a technique called immunofluorescence9 to visualize the cells in the tissue including pyramidal neurons10, dentate granule neurons11, and astrocytes12.
- Pyramidal neurons are involved in memory and communicate with other regions of the brain.
- Dentate granule (DG) neurons send and receive messages from other brain regions. The most important messages will get passed on to pyramidal neurons. The less important messages are filtered out by the DG neurons and do not get passed on. In people with epilepsy, DG neurons no longer filter messages as well, leading to memory issues and seizures.
- Astrocytes are a type of brain cell that support neurons by providing nutrients and repairing cell damage.
Olivia used fluorescent proteins to label the cells in the hippocampus. All cells were labeled with a blue, fluorescent protein marker called 4′,6-diamidino-2-phenylindole (DAPI). A second fluorescent marker was used to label a protein found only in astrocytes, called glial fibrillary acidic protein (GFAP). Under healthy conditions, astrocytes do not produce a detectable amount of GFAP. However, when the tissue starts to get inflamed, astrocytes try to help by increasing production of GFAP. Astrocytes labeled in green express lots of GFAP and are a marker of inflammation.
Visualizing the hippocampus tissue in this way, Olivia could clearly see that the brains of the control mice after 2 months were clearly inflamed compared to the treatment group and the mice without epilepsy.

Figure 2.
The brains of control mice with epilepsy have increased levels of inflammation, indicated by the increased expression of GFAP (green) in astrocytes.
[Source: Roopra Lab]
Preliminary follow-up studies suggested that mice in the drug-treated group remain protected up to 4 months after treatment with tofacitinib. “This was a really big deal,” Dr. Roopra emphasized. “This medication is attacking some fundamental mechanism causing epilepsy.”
The researchers also conducted behavioral experiments on the mice to assess their cognition while exploring a maze in the shape of a Y, called a Y maze.

Figure 3.
Mouse navigating a Y maze to assess its cognition.
[Source: Roopra Lab]
In mice whose seizures stopped after treatment with tofacitinib, their cognitive function was almost completely restored. With this restored cognitive function, the researchers also saw signs of decreased inflammation in the brain. A colleague in a different lab repeated the same experiments and got similar results. “We are really excited about where this might take us,” Dr. Roopra commented.
Olivia and Dr. Roopra are conducting ongoing experiments to better understand how tofacitinib is impacting neurons in mice with epilepsy. “We saw this dramatic effect, but we still don’t really know why,” said Dr. Roopra. The researchers are building cellular and molecular models to help them understand. Olivia is also sifting through large datasets to see which genes did not go back to normal with the medication and how those genes might be targeted with a combination of treatments. Ultimately, the researchers hope to test tofacitinib in clinical trials13 of patients with epilepsy.
To Dr. Roopra and Olivia, the moral of the story is: follow the data. “This project could have gone a lot of different ways,” recalled Olivia, “We followed what the data told us, and we ended up in this really unexpected direction.” The researchers also emphasize the role of math in research and life sciences. “Bringing mathematics into the life sciences is how we are going to make the scientific discoveries of the future,” concluded Dr. Roopra.
Dr. Avtar Roopra is Professor of Neuroscience at the University of Wisconsin, Madison. His research focuses on understanding the genetic changes underlying epilepsy and cancer with the goal of developing improved treatment options. When not in the laboratory, Dr. Roopra enjoys building and flying model airplanes, spending time with friends and family, and looking up at the stars.
Dr. Olivia Hoffman is a post-doctoral researcher in Dr. Roopra’s lab, where she studies the genetic changes underlying the development of epilepsy. She graduated with her PhD in January 2025, and the research described here was part of her doctoral work. When not in the laboratory, Dr. Hoffman enjoys running, woodworking, painting, and spending time with friends and family.
For More Information:
- Hoffman OR, Koehler JL, Espina JEC, Patterson AM, Gohar ES, Coleman EM, Schoenike BA, Espinosa-Garcia C, Paredes F, Varvel NH, Dingledine RJ, Maguire JL, Roopra AS. Disease modification upon 2 weeks of tofacitinib treatment in a mouse model of chronic epilepsy. Sci Transl Med. 2025 Mar 19;17(790):eadt0527. https://www.science.org/doi/10.1126/scitranslmed.adt0527
- Roopra Lab Discovers Arthritis Drug Provides Effective Epilepsy Treatment in Mice
https://neuro.wisc.edu/2025/03/26/roopra-lab-discovers-arthritis-drug-provides-effective-epilepsy-treatment-in-mice/
To Learn More:
- Avtar Roopra’s Lab. https://576192955820480192.weebly.com
- National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/health-information/disorders/epilepsy-and-seizures
- Epilepsy Foundation. https://www.epilepsy.com/what-is-epilepsy
- American Association of Neurological Surgeons. https://www.aans.org/patients/conditions-treatments/epilepsy/
Written by Rebecca Kranz with Andrea Gwosdow, PhD at www.gwosdow.com