Highlights
Diabetes is a chronic medical condition characterized by the body’s decreased ability to utilize sugar. If diabetes is not controlled, it can lead to complications including delayed wound healing and nerve damage of the corneas.
These researchers compared the epigenetic changes in gene expression in the corneas of people with and without diabetes. In diabetic corneas, they found altered expression of the WNT5A gene, which encodes the cell signaling protein Wnt-5a.
The researchers used three interventions to promote wound healing in a model of corneal epithelial cells. All three methods worked. In the future, they plan to test these treatments in combination to see if they can promote faster wound healing. They are also studying the mechanism of action of Wnt-5a to learn more about how it works to promote wound healing in the diabetic cornea.
Did you know that the
corneas
of the eye are the organs with the greatest number of nerves in the body? The cornea is the outermost covering of the eye and is essential to clear vision because it bends light as it enters the eye, allowing you to focus. It also protects the eye by filtering out dirt, germs, and some UV light. The high density of corneal nerves allows us to see clearly but also makes the corneas particularly susceptible to nerve damage.
One common cause of nerve damage in the eye is
diabetes,
a chronic medical condition characterized by changes in the body’s ability to utilize sugar.
Diabetic eye disease
affects many parts of the eye, including the cornea. Dr. Alexander Ljubimov, Professor of Neurosurgery and Biomedical Sciences and Director of the Regenerative Medicine Institute Eye Program at Cedars-Sinai Medical Center, Los Angeles, California has dedicated much of his research career to better understanding corneal disease in people with diabetes and developing new treatment options. In a recent study, Dr. Ljubimov and his team, including research scientist Dr. Ruchi Shah, have identified cellular changes in the corneas of people with diabetes and tested novel treatments to improve corneal function.
An Epidemic of Diabetes
According to the National Institute of Diabetes and Digestive and Kidney Disorders approximately 37 million Americans have been diagnosed with diabetes, including 283,000 young adults under 20 years of age. There is currently no cure for diabetes, but diet, exercise, and medications can help keep blood sugar controlled and avoid complications. Common complications of uncontrolled diabetes include
heart disease,
kidney disease,
neuropathy,
and diabetic eye disease.
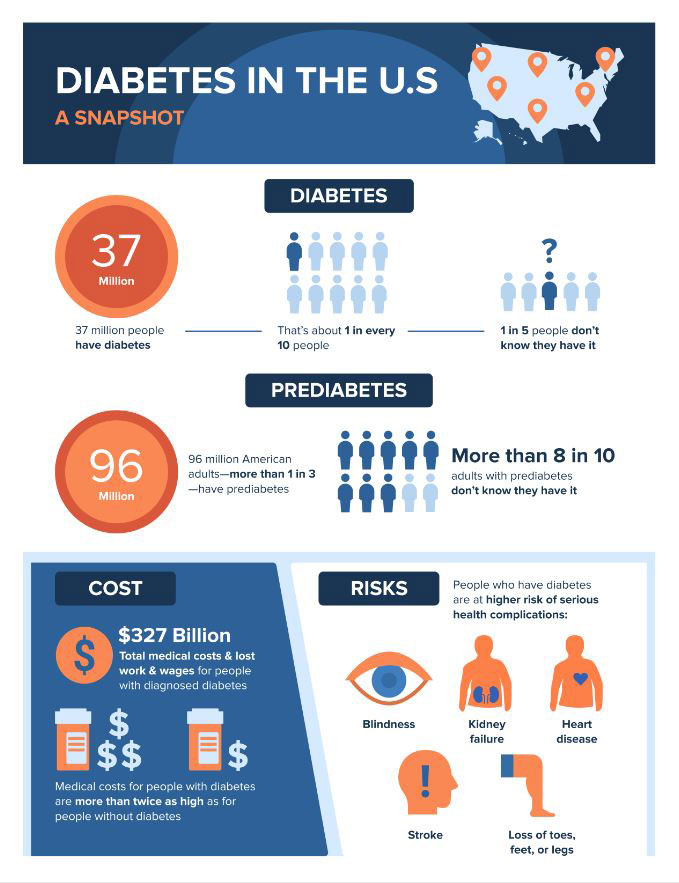
Figure 1. Statistics about diabetes in the United States.
[Source: https://www.cdc.gov/diabetes/library/socialmedia/infographics/diabetes.html]
Previous What A Year! articles have discussed a variety of research topics related to understanding diabetes, improving treatment options, and reducing complications. For example, How to Program Stem Cells from June 2022 highlighted the work of Dr. Douglas Melton to develop stem cell therapy for people with type 1 diabetes. The Science of Cinnamon from February 2018 described the work of Dr. Amy Stockert on the role of cinnamon in controlling blood sugar. This article will focus on the understanding and treatment of a specific complication of diabetes: diabetic
corneal disease.
From Gene to Protein
Each of our cells in every organ of the body contains the exact same genetic information that provides the instructions for building the proteins that allow our tissues and organs to function. This information, encoded in
deoxyribonucleic acid
(DNA), leads to
protein synthesis
through complex processes typically divided into two parts:
transcription
and
translation.
These processes are briefly summarized here to better understand the cellular changes identified in this research.
DNA and its encoded information must remain in the
nucleus
of the cell. Protein synthesis occurs outside of the nucleus in the
ribosomes.
During transcription, DNA is copied or “transcribed” into
ribonucleic acid
(RNA), which leaves the nucleus and transfers the information to the ribosomes. During translation, RNA is used as a template to create proteins. Although all our cells have the exact same DNA, each organ in the body has its own ways of transcribing the same genetic information into the different proteins it needs to function.
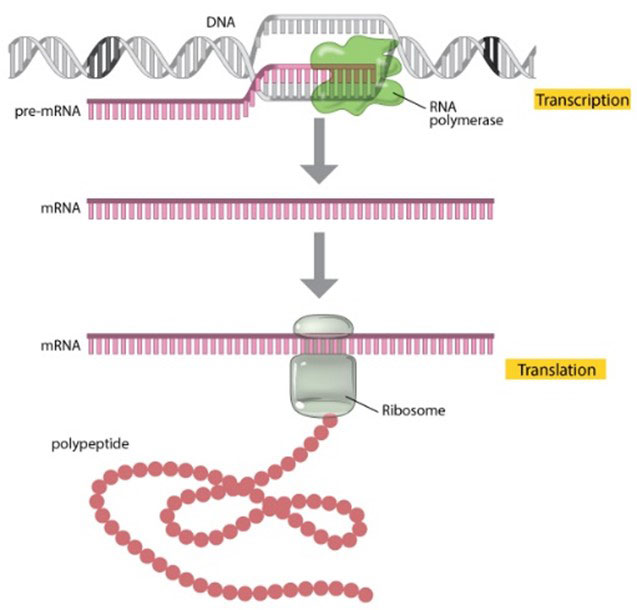
Figure 2. Transcription and translation lead to protein synthesis.
[Source: https://www.nature.com/scitable/topicpage/translation-dna-to-mrna-to-protein-393/]
A gene and the protein it encodes often have the same name but are distinguished by their formatting. For example, in the research described here, Dr. Ljubimov, Dr. Shah, and colleagues focused on the gene WNT5A that encodes the protein Wnt-5a.
Transcription and translation are tightly regulated by a variety of molecules that control when protein synthesis begins and how many proteins are produced. It is possible to alter protein synthesis without changing the underlying genetic information by affecting these processes. This kind of change is called
epigenetics.
Epigenetic changes can occur through several distinct mechanisms. For example, they can halt transcription by modifying the DNA such that the enzymes involved in transcription don’t recognize it or can’t bind to it. This process, called
DNA methylation,
happens when a methyl group (one carbon and three hydrogen atoms) is added to the area of the DNA that marks where transcription begins. Another type of epigenetic change occurs through
microRNA
(miRNA). miRNAs are small RNA molecules that can destabilize RNA so that the encoded protein cannot be synthesized.
Diabetic Corneal Disease
One way that diabetes affects the body is through these epigenetic changes. Such changes have been described in other organs of the body in people with diabetes. In this research, Dr. Ljubimov, Dr. Shah, and colleagues investigated epigenetic changes in the corneas of people with diabetes.
The cornea is a tough, transparent tissue that contains five layers including the
epithelium,
the outermost layer, which is constantly exposed to the external world.
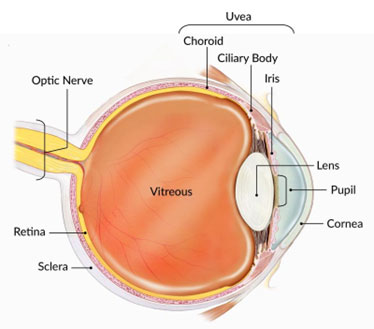
Figure 3. The cornea and other parts of the eye.
[Source: https://www.nei.nih.gov/learn-about-eye-health/healthy-vision/how-eyes-work]
Old corneal epithelial cells are regularly replaced by new ones. These cells are derived from
limbal epithelial stem cells,
precursor cells residing at the periphery of the epithelium until they are needed.
Figure 4. Limbal epithelial cells enriched in stem cells.
[Source: Dr. Ljubimov]
As the outermost part of the eye, the cornea is prone to injury. Since the cornea plays an integral part in clear vision, damage to the cornea can lead to changes in vision and vision loss. One common type of corneal injury is a scratch or abrasion. This happens when a disruption of the cornea causes damage to the epithelium.
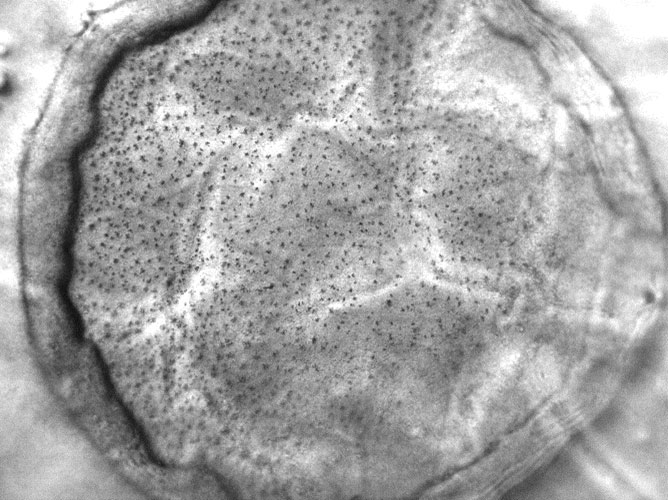
Figure 5. Cornea after 2 days of injury. The center of the ring has been wounded.
[Source: Dr. Ljubimov]
The American Academy of Ophthalmology lists fingernails, makeup brushes, and tree branches as common causes of
corneal abrasions.
When a healthy cornea is injured, limbal epithelial stem cells are stimulated to become corneal epithelial cells and replace the damaged tissue.
Diabetes can cause a variety of changes in the cornea including incomplete wound healing and nerve damage. An estimated 45-70% of people with diabetes experience some kind of corneal complications. Problems with the cornea are often underdiagnosed in people with diabetes because the changes can be subtle unless the cornea is damaged. Symptoms of corneal damage include pain, irritation, dryness in the eye, and cloudy or blurry vision. Dysfunction of the limbal epithelial stem cells due to diabetes delays healing of the cornea, meaning that these uncomfortable symptoms are prolonged.
Identifying Epigenetic Changes in Diabetic Corneas
To better understand what was happening at the epigenetic level in the limbal epithelial stem cells of diabetic corneas, Dr. Ljubimov and Dr. Shah compared the epigenetic profile of corneal cells in people with and without diabetes. Specifically, the researchers looked at differences in DNA methylation that would indicate epigenetic changes in diabetic corneas. They identified a specific gene, WNT5A, which was hypermethylated in diabetic corneas. “This was an exciting finding because Wnt-5a is part of a group of signaling molecules involved in many cellular processes related to wound healing, including stem cell maintenance and cell growth,” commented Dr. Shah. The researchers also observed an increase in miRNA that inhibits Wnt-5a expression.
This discovery led to follow-up experiments to identify any changes in protein expression as a result of WNT5A hypermethylation. These experiments confirmed that synthesis of Wnt-5a was reduced in diabetic corneas. “These results are similar to epigenetic changes due to diabetes that have been demonstrated in other organs,” added Dr. Ljubimov. “This was the first time these changes had been reported in the corneas of people with diabetes.”
Treating Diabetic Corneal Disease
The goal of Dr. Ljubimov’s research into epigenetic changes in diabetic corneas is to develop treatments to reverse these effects. To test possible treatment methods, Dr. Ljubimov, Dr. Shah, and colleagues created two systems of model corneas. In the first model, limbal epithelial stem cells were grown in a petri dish until they completely covered the dish. The researchers used a pipette to create a wound in these cells and measured the time it took for the wound to heal. In the second system, whole corneas dissected from donated eyes were maintained in a petri dish and the corneal epithelium was wounded using a chemical known as 1-heptanol. These were the control conditions.
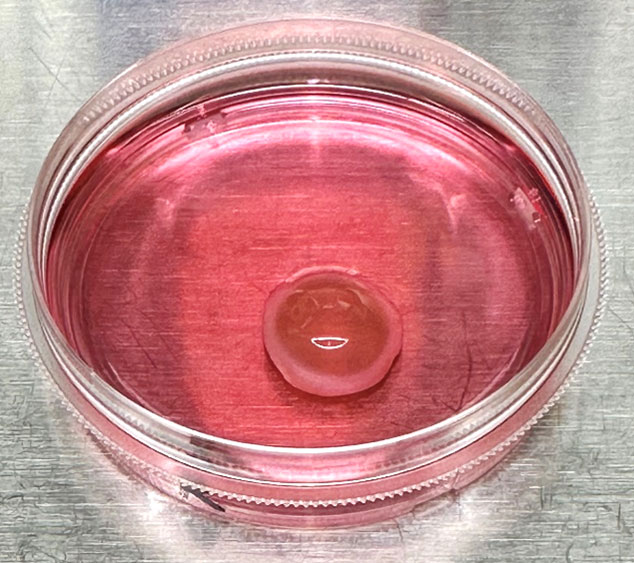
Figure 6. The method of maintaining a cornea in a petri dish is known as corneal organ culture.
[Source: Dr. Ljubimov]
The researchers used three distinct interventions to promote wound healing. First, they added the Wnt-5a protein directly to the cells. Second, they used the molecule zebularine, which is known to block DNA methylation. Third, they used a nano drug developed in Dr. Ljubimov’s laboratory to silence the miRNA that was increased in diabetic corneas. All three of the treatment methods worked to reduce wound healing time in both model systems.
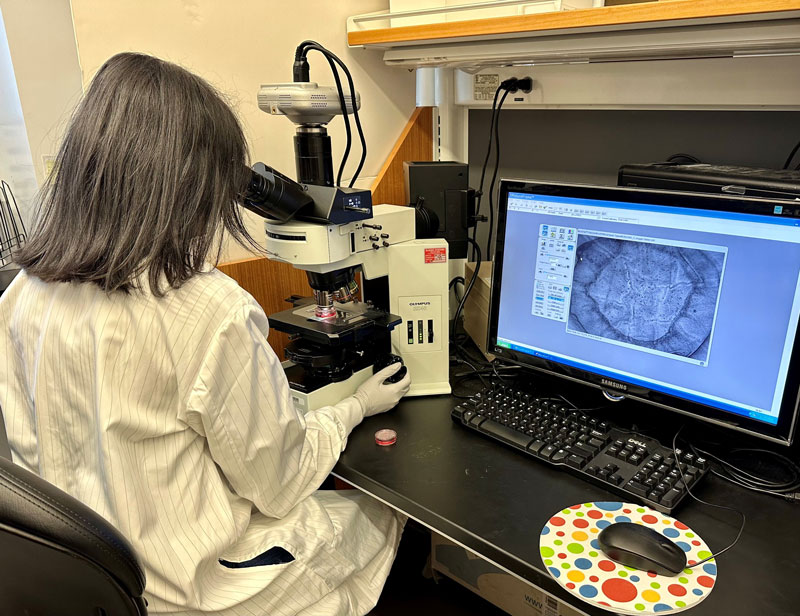
Figure 7. Dr. Shah monitoring the wound healing process of a diabetic cornea.
[Source: Dr. Shah]
In future research, Dr. Ljubimov, Dr. Shah, and colleagues plan to test the treatment options in combination to see if they can promote faster wound healing. They are also actively studying the mechanism of action of Wnt-5a to learn more about how it works to promote wound healing in the cornea.
High School Student-Researchers
This project was conducted with the help of two high school students, Connie Lim and Shweta Jinka. Connie and Shweta had the opportunity to spend the summer working with Dr. Ljubimov and Dr. Shah in the lab as part of the California Institute for Regenerative Medicine’s Summer Program to Accelerate Regenerative Medicine Knowledge for high school students. Connie assisted Dr. Shah in testing possible treatment options for wound healing. Shweta worked on an ongoing project to better understand the mechanisms of action of Wnt-5a. “Research is a great field, and you should definitely try it if you’re interested,” Connie commented. “I learned that research is very collaborative and involves many different people,” added Shweta. Connie is now a senior at Palos Verdes High School in Palos Verdes Estates, CA. Shweta is now a senior at Valencia High School in Valencia, CA.
Dr. Ruchi Shah is a research scientist in the laboratory of Dr. Alexander Ljubimov at Cedars-Sinai Medical Center in Los Angeles, CA. Her research focuses on DNA methylation patterns in diabetic corneas and the role of Wnt-5a signaling in corneal wound healing. Outside of the laboratory, Dr. Shah enjoys landscape painting.
Dr. Alexander Ljubimov is Professor of Neurosurgery and Biomedical Sciences and Director of the Regenerative Medicine Institute Eye Program at Cedars-Sinai Medical Center. His research focuses on the impact of diabetes on the corneas. When not in the laboratory, Dr. Ljubimov enjoys reading, photography, and visiting museums.
For More Information:
- Shah, R. et al. 2023. “Reversal of dual epigenetic repression of non-canonical Wnt-5a normalises diabetic corneal epithelial wound healing and stem cells.” Diabetologia, 66:1943-58. https://link.springer.com/article/10.1007/s00125-023-05960-1
- Shah, R. et al. 2021. “Systemic diseases and the cornea.” Exp Eye Res, 204:108455. https://www.sciencedirect.com/science/article/pii/S0014483521000208?via%3Dihub
- Saghizadeh, M. et al. 2017. “Concise review: stem cells for corneal wound healing.” Stem Cells, 35(10): 2105-2114. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5637932/
To Learn More:
Diabetes
- “Diabetes.” Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/index.html
- “What is diabetes?” National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes
Corneal Diseases
- “Corneal Conditions.” National Eye Institute. https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/corneal-conditions
- “Corneal Disorders.” National Library of Medicine. https://medlineplus.gov/cornealdisorders.html
Epigenetics
- “What is epigenetics?” Centers for Disease Control and Prevention. https://www.cdc.gov/genomics/disease/epigenetics.htm.
- “Epigenetics.” National Human Genome Research Institute. https://www.genome.gov/genetics-glossary/Epigenetics
Written by Rebecca Kranz with Andrea Gwosdow, PhD at www.gwosdow.com
HOME | ABOUT | ARCHIVES | TEACHERS | LINKS | CONTACT
All content on this site is © Massachusetts
Society for Medical Research or others. Please read our copyright
statement — it is important. |

