Highlights
Cancer is a class of diseases characterized by abnormal tissue growth. These researchers developed a novel noninvasive treatment for treating cancer using high intensity sound waves known as histotripsy. Studies in rodent models have shown that partial treatment with histotripsy can cause the complete regression of liver tumors. Early-stage clinical trials also show promising results.
The researchers hope that histotripsy can be a life-saving treatment for cancer patients. They continue to test the treatment in different types of cancers as well as other conditions and diseases characterized by abnormal or unwanted tissue growth.
What comes to mind when you think of cancer treatment? Chemotherapy, radiation, and surgery are all common types of treatments for cancer, though specific treatment plans will vary depending on the type and stage of cancer, among other variables. New research by Drs. Zhen Xu and Tejaswi Worlikar demonstrates the possibilities for a new, noninvasive treatment from an unlikely source: high-intensity sound waves. Collaborators include Drs. Timothy Hall, Man Zhang, Anutosh Ganguly, Clifford Cho, Mishal Mendiratta Lala, Lili Zhao, and Jiaqi Shi at the University of Michigan and Dr. Fred Lee at the University of Wisconsin.
Acoustic Cavitation and Histotripsy
As humans, we breathe in oxygen and exhale carbon dioxide. As a result, our blood and tissues are filled with
nanometer-sized
gas particles. When these particles are exposed to high-intensity sound waves, the bubbles expand and then explode, resulting in surrounding cells being torn apart. This process is called
acoustic cavitation.
As a graduate student, Dr. Zhen Xu worked in a laboratory that studied how acoustic cavitation works and potential therapeutic possibilities. Scientists had known about acoustic cavitation since the development of ultrasound technology, which uses sound waves to create images of tissues and organs. However, acoustic cavitation was thought to be an uncontrollable and potentially dangerous process that should be avoided during treatment.
Drs. Zhen Xu, Charles Cain, Timothy Hall, and Brian Fowlkes turned scientific understanding of acoustic cavitation upside down by developing a novel treatment called
histotripsy.

Figure 1. Video explaining histotripsy treatment.
[Source: University of Michigan Histotripsy Group. https://histotripsy.umich.edu/]
The word “histotripsy” comes from the Greek “histo” meaning soft tissue and “tripsy” meaning breakdown. Histotripsy uses high-intensity sound waves to break down soft tissue in a targeted way. The device used to deliver histotripsy is called an ultrasound
transducer.
It looks like the same type of machine used during ultrasound exams, like those used to take pictures of one’s internal organs.
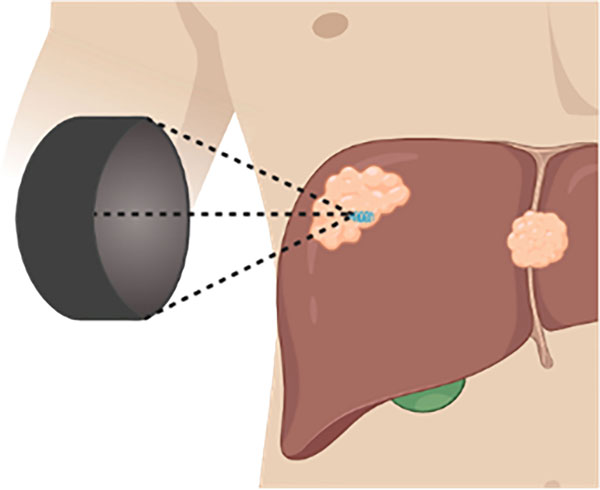
Figure 2. Image of transducer providing histotripsy treatment.
[Source: Hendricks-Wenger et al, 2022, Figure 4: https://www.frontiersin.org/articles/10.3389/fonc.2021.681629/full]
Whereas ultrasound equipment used clinically delivers low intensity sound waves, the histotripsy transducer is designed to deliver very high intensity sound waves.

Figure 3. Video of what histotripsy treatment looks like at the cellular level.
[Source: University of Michigan Histotripsy Group. https://www.youtube.com/watch?v=WS_VzTLRU8Y]
Histotripsy is completely noninvasive, targeting a specific part of the body from the outside with large bursts of energy.
Histotripsy as Potential Cancer Treatment
Dr. Xu and colleagues hypothesized that histotripsy could be used to treat a variety of conditions characterized by unwanted or unhealthy tissue. First, they had to perfect the technique on normal, healthy tissue. They conducted experiments to determine the optimal intensity and dosage of sound waves for tissue breakdown. They also tested different organs and tissue areas to see in which areas of the body and how far below the skin the process could be successful.
Once Dr. Xu and colleagues optimized the histotripsy treatment on healthy tissue, they turned to cancerous tissue. Cancer is a disease characterized by uncontrolled tissue growth, and the researchers were eager to see whether histotripsy might offer a potential noninvasive treatment option.
To begin, Dr. Xu and colleagues started with mouse models that had tumors located just under the skin surface, known as
subcutaneous
tumors. The mouse models were
immunodeficient,
meaning that they did not have a functioning immune system. Dr. Xu and her graduate student, Tejaswi Worlikar, chose an immunodeficient mouse model to be able to generate and treat human-derived liver tumors in mice and study how they responded to histotripsy. Five weeks after the tumors were treated with histotripsy, Dr. Xu and Tejaswi observed that the subcutaneous tumors started to regress, or decrease, in size. This was a promising initial result.
One limitation of a subcutaneous tumor model is that total ablation (destruction) of the tumor is not possible. This is because complete treatment of the tumor would also destroy the skin. As a result, some part of the tumor had to be left during these experiments, and the subcutaneous tumor would grow back.
To address this limitation, Dr. Xu and Tejaswi moved to a model of rodent liver cancer, in which tumors were located within the liver. The researchers chose liver cancer because it has one of the lowest survival rates of all types of cancer in the United States. This time the researchers used
immunocompetent
rat models that had intact immune systems. They used histotripsy to perform complete ablation of the liver tumor, meaning the entire tumor was targeted and destroyed. The results of the study showed tumor regression in all tumors targeted completely.
Next, Dr. Xu and Tejaswi wanted to test the effects of partial ablation with histotripsy compared to complete ablation.
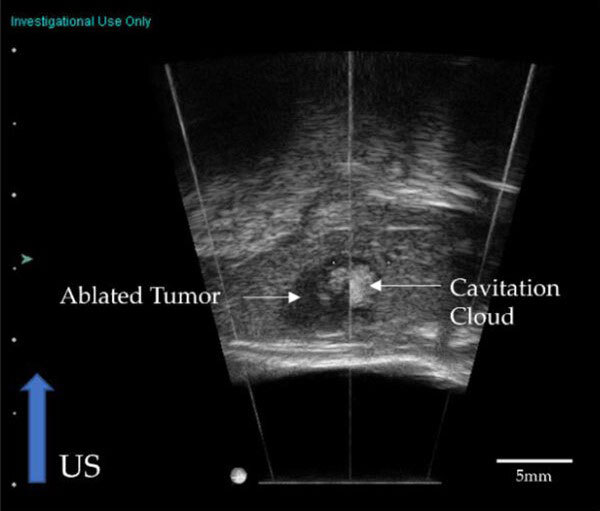
Figure 4. Ultrasound image of cavitation cloud during partial ablation of a liver tumor.
[Source: Worlikar et al, 2022, Figure 1b]
Partial ablation means that only some of the tumor tissue was targeted and destroyed. The researchers were interested in partial ablation because complete ablation may not be possible in some clinical situations, such as if tumors are located near vital organs or critical structures. In addition, it is important to know the treatment response if a tumor is left partially untreated, especially because some techniques that use partial ablation can cause tumors to grow back more aggressively. This possibility increases the risk of using such techniques.
The researchers wanted to know whether histotripsy might cause undesirable effects in targeted tumors. After completing the experiments, the researchers observed regression in 5 out of 6 animals in this study, and the tumor continued to grow in 1 out of 6 animals. No regrowth in regressed tumors was observed.
In a follow-up experiment to look at partial ablation more closely, complete regression was observed in 9 out of 11 animals. “Even though we only destroyed 50-75% of the liver tumor, we saw that 100% of the tumor disappeared from the animal three weeks following treatment,” explained Tejaswi. “This is an exciting result because it shows that it may be possible to cause complete regression in tumors that can only be partially ablated.”
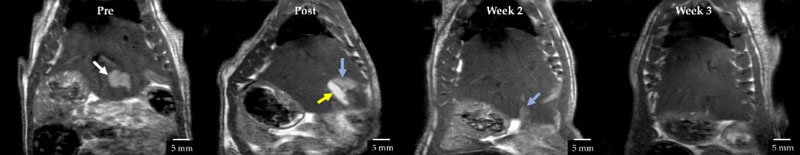
Figure 5. Tumor regression after treatment with histotripsy. Prior to treatment, the tumor is indicated by a white arrow. Over the course of three weeks, the tumor completely regresses.
[Source: Worlikar et al, 2022, Figure 3b]
Dr. Xu and Tejaswi hypothesize that partial ablation may lead to total tumor regression due to the involvement of the immune system. “We think that somehow, after treatment with histotripsy, the immune system is activated to clean up the area and destroy the remaining tumor cells,” added Tejaswi.
Ongoing Clinical Trials
In order to bring her findings from the laboratory towards clinical use, Dr. Xu had co-founded the company Histosonics. Histosonics has developed a histotripsy system called EdisonTM that is currently being studied in Phase 3 clinical trials to determine how it compares to other treatment options at sites across Europe and the United States. The trial is called
“The HistoSonics System for Treatment of Primary and Metastatic Liver Tumors Using Histotripsy”
or HOPE4LIVER for short. The study has recently completed patient enrollment. In order to be eligible to participate, patients must meet certain criteria specific to their liver and kidney function and their diagnosis such as the size of the liver tumor. In addition, only patients who have not responded to or been intolerant of other currently available treatments are allowed to participate.
Participants in the clinical trial undergo histotripsy treatment followed by imaging studies within 36 hours to determine how well the treatment targeted the tumor tissue. Patients are followed for 30 days after treatment to better understand the results.
In a case report published from an earlier Phase 1 clinical trial at a research site in Spain, the authors described one patient with multiple tumors in the liver. Only one of the tumors was treated with histotripsy, yet clinicians observed a reduction in tumor growth across all liver tumors. They also observed a reduction in cancer markers overall. “The clinical trials are still ongoing,” Tejaswi commented, “but these are promising results.”
Future Work
Based on the results of the experiments and clinical trials described here, Drs. Xu and Cho hypothesize that histotripsy treatment activates an immune response. In future research, Dr. Xu, Tejaswi, and their collaborators plan to study the mechanisms of this response further. In addition, the researchers want to conduct similar experiments in models of different types of cancer to determine whether their results are specific to only liver cancer or if the results can be applied more broadly to other types of cancers.
Tejaswi Worlikar conducted the research described in this article while a graduate student in the laboratory of Dr. Zhen Xu. She graduated recently and is continuing her work in Dr. Xu’s laboratory as a post-doctoral fellow. When not in the laboratory, Dr. Worlikar enjoys reading, painting, and spending time with her dog and cat.
Dr. Zhen Xu is Professor of Biomedical Engineering at the University of Michigan. Her research focuses on the use of histotripsy as a possible therapeutic intervention for a variety of conditions including cancer. When not in the laboratory, Dr. Xu enjoys biking, running, paddle boarding, and reading.
For More Information:
- Worlikar, T. et al. 2022. “Impact of Histotripsy on Development of Intrahepatic Metastases in a Rodent Liver Tumor Model.” Cancers, 14(7). https://www.mdpi.com/2072-6694/14/7/1612
To Learn More:
- Xu Laboratory, Histotripsy Group. https://histotripsy.umich.edu/
- “Introduction to Histotripsy” webinar with Dr. Fred Lee. https://zoom.us/rec/play...
- #HOPE4LIVER US Clinical Trial. https://clinicaltrials.gov/ct2/show/NCT04572633?cond=hope4liver&draw=2&rank=2
- Histosonics. https://histosonics.com/the-science/
Written by Rebecca Kranz with Andrea Gwosdow, PhD at www.gwosdow.com
HOME | ABOUT | ARCHIVES | TEACHERS | LINKS | CONTACT
All content on this site is © Massachusetts
Society for Medical Research or others. Please read our copyright
statement — it is important. |

