Highlights
Massage is an ancient therapeutic practice that can support healing and pain relief in a variety of conditions. It has been difficult for researchers to study the specific mechanisms and effects of massage due to the multitude of massage techniques and differences between specific practitioners. These researchers designed a robotic system to deliver mechanical stimulation (a specific form of massage) that could be controlled and measured. The results showed that this system can improve muscle function in injured mouse muscles compared to controls. Moreover, the researchers showed the robotic system was effective because it helps remove immune cells, specifically neutrophils, from the injured site.
Next steps for the research include repeating similar experiments in larger animal models, such as rabbits and pigs.
A massage can be a healing salve for sore and stressed muscles. New research by Dr. Bo Ri Seo and colleagues in the Mooney Laboratory at the Wyss Institute for Biologically Inspired Engineering at Harvard University shows that massage can do more than just feel good – it can actually help muscles heal faster.
Muscle Injury and Repair
Skeletal muscle
cells consist of multiple
muscle fibers
that work together to create force and movement.
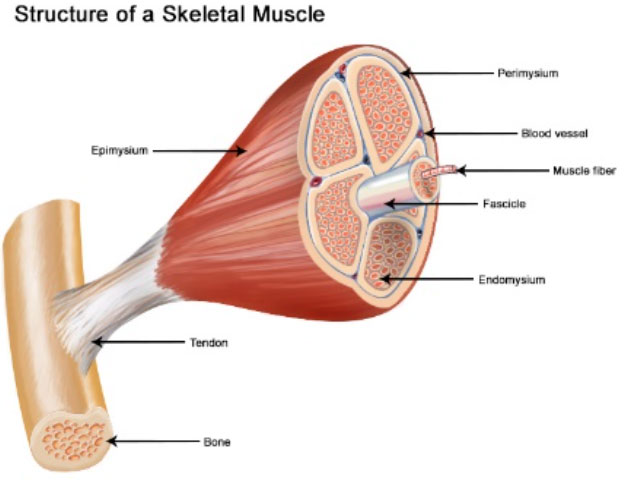
Figure 1. Structure of skeletal muscle
[Source: https://training.seer.cancer.gov/anatomy/muscular/structure.html]
There are two main types of muscle fibers in any given muscle: Type 1 and Type 2. Type 1 muscle fibers are resistant to fatigue. These are the types of muscle fibers that endurance athletes need to strengthen. Type 2 muscle fibers can exert higher forces. These are the types of muscle fibers that speed athletes need to strengthen.
Each muscle tissue (for example, biceps, abdominal, calf muscles, etc.) has its own specific composition of muscle fiber types, which determines the physical characteristics and performance of each muscle tissue (Peiseler and Kubes, 2019). However, the composition of muscle fiber types can be changed by physical training, aging or illness (Tidball, 2017).
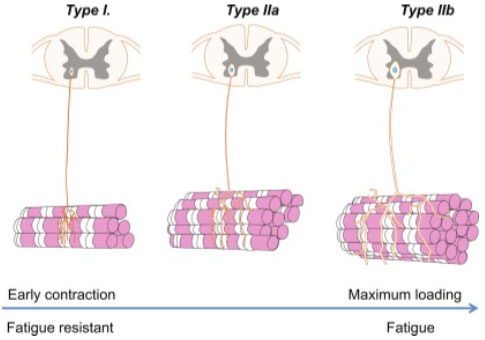
Figure 2. Types of muscle fibers in humans
[Source: https://www.sciencedirect.com/topics/medicine-and-dentistry/fast-muscle-fiber]
When a muscle is injured, the composition and contractility of muscle fibers is affected. Under a microscope, injured muscle has many dead muscle fibers, large numbers of
immune
cells, and
muscle fibrosis.
Immune cells are present in injured muscle because the immune system is actively involved in tissue repair after an injury. The immune system is a network of cells, tissues, and organs that work together to prevent disease, fight infection, and repair damaged tissue.
White blood cells
are a type of immune cell often present during tissue repair. There are many types of white blood cells including
macrophages
and
neutrophils.
Macrophages engulf and destroy infected or damaged cells.
Neutrophils are one of the first responders of the immune system. Since they are highly mobile, they are instantly recruited to the infected or injured site in response to signals from pathogens and dead or damaged cells to remove them (Mann et al. 2011).
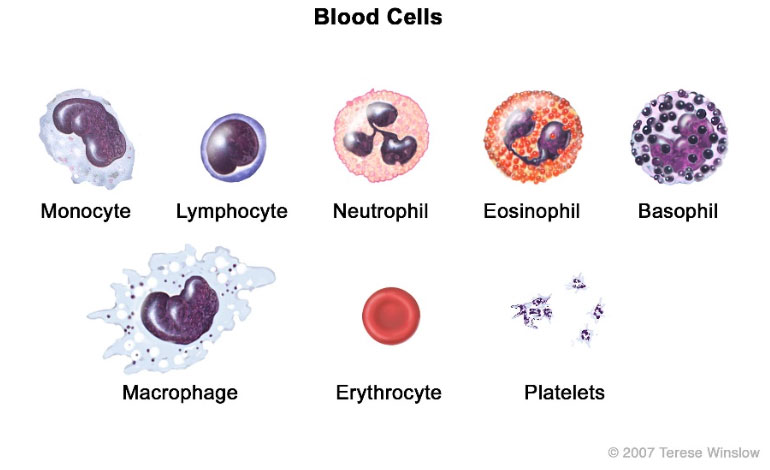
Figure 3. Types of blood cells including neutrophils and macrophages
[Source: https://www.cancer.gov/publications/dictionaries/cancer-terms/def/macrophage]
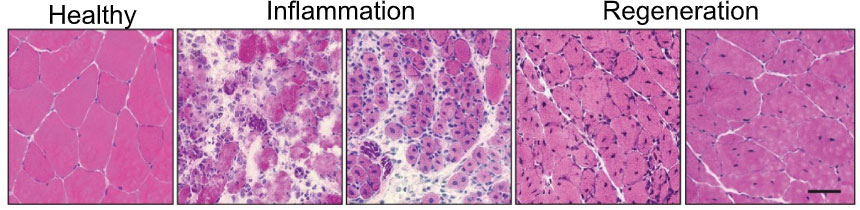
Figure 4. Images of mouse muscle tissue when healthy, with inflammation, and in the process of healing (regeneration)
[Source: Mann et al. 2011]
As a result, the muscle fibers are weakened. As an injury heals, the dead muscle fibers are cleared and replaced with new ones, and muscle fibrosis should also be resolved. However, if an injury doesn’t heal fully, the muscle fibers can remain in this weakened and less functional state of fibrosis. It is important to keep muscle tissue active after injury to avoid fibrosis and improve healing. This is where massage comes in.
Massage is an ancient practice developed in many cultures around the world to ease muscle tension and improve blood flow. In the United States, massage therapy practiced by a licensed massage therapist has been found to be helpful in some patients with cancer, chronic headaches, and muscle and joint problems. One big challenge to knowing whether and how effective massage therapy can be is that each massage therapist practices differently, using different techniques, and different force. With so many variables from patient to patient, it has been difficult for researchers to make comparisons and draw conclusions about the effectiveness of a given massage technique.
Developing a Robotic Device
In order to solve this problem, Dr. Seo and her colleagues set out to design a controlled and reproducible experiment that would allow them to better understand whether and how muscle recovery was impacted by massage. Dr. Seo partnered with Dr. Chris Payne and colleagues in the Harvard Biodesign Lab run by Professor Conor Walsh to develop a robotic machine that could provide mechanical stimulation to the injured hindlimb of a mouse. Mechanical stimulation is a more precise word to describe the type of massage the robotic device delivered to the muscle. The robotic device wrapped around the hindlimb of the mouse and caused muscle compression and release at a steady cyclical rate that the researchers could control and measure.
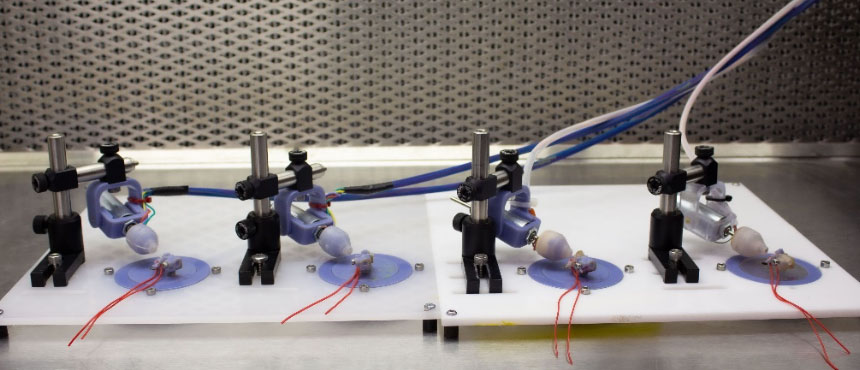
Figure 5. Robotic device to deliver mechanical stimulation, designed by Dr. Seo, Dr. Payne, and colleagues
[Source: Harvard University and Wyss Institute]
It took several attempts and revisions of the robotic device until it worked well enough to provide consistent cyclical mechanical stimulation needed for reproducible experiments. Once the device was working properly, Dr. Seo and her colleagues tested different parameters of their intervention with mechanical stimulation. For example, after observing the effects of consistent mechanical stimulation over 3, 7, 14, and 21 days, the researchers determined that 14 days of treatment was sufficient for maximal effect. In addition, the researchers found the ideal range of force the robot needed to provide to the muscles was between 0.15 and 0.6
Newtons.
Anything less than 0.15 Newtons had no effect compared to the untreated control group, and more than 0.6 Newtons caused visible damage to the skin and tissue. For comparison, one Newton of force is approximately the force exerted by a medium-sized apple as you hold it in your hand. Finally, Dr. Seo and her team tested the ideal amount of muscle strain, a value that can be used to compare the amount of mechanical stimulation across muscles of different sizes. The researchers found the optimal percentage of muscle strain was 10-40% compression.
During these initial tests, Dr. Seo and colleagues used ultrasound to visualize exactly what was happening as the muscles were compressed by the robotic device.
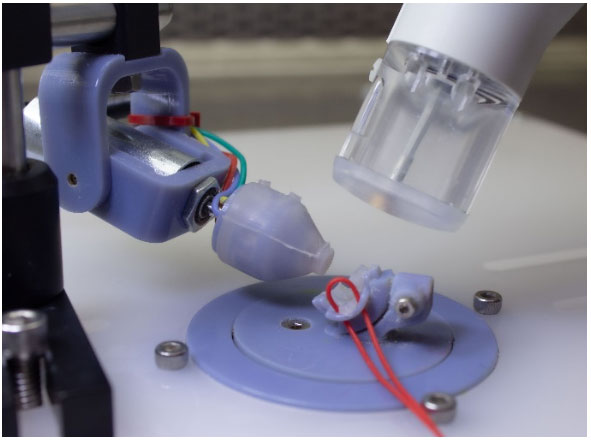
Figure 6. Close-up view of robotic device with ultrasound
[Source: Harvard University and Wyss Institute]
The researchers used the criteria described above to develop a computational model. This model will be used in future experiments with other animals and other body parts to determine, for example, the specific amount of force needed to achieve a target percentage of muscle compression. “It was really exciting for us to be able to develop this model,” Dr. Chris Payne commented. “It supports our goal of measuring specific parameters of massage to achieve the most effective muscle recovery.”
Experimental Results
In an initial series of experiments, Dr. Seo and her colleagues exposed mice with muscle injury in their hindlimb to five minutes of robotic mechanical stimulation every 10-12 hours for 14 days. The researchers compared three different treatment groups with different amounts of force: 0.15N, 0.3N, and 0.6N.
To assess the effectiveness of the treatment, Dr. Seo and colleagues measured muscle fiber composition, contractile force, and fibrosis in the injured muscle compared with healthy, uninjured mice and injured mice who did not receive treatment. “These results were quite surprising,” recalled Stephanie McNamara, co-author and doctoral student in the Mooney lab. “We found that in all three experimental groups, the injured muscle had even greater contractile force than the uninjured muscle of the control mice, about 1.5 to 2 times the functional improvement.” In fact, the amount of improvement observed was similar to that seen by other researchers who exposed injured mice to stem cells or other biological treatments.
Clearly the robotic mechanical stimulation was having a positive effect on the injured muscle tissue, and it was doing so in a noninvasive way. Next, Dr. Seo and her colleagues wanted to figure out why they were seeing such profound results.
Since muscle recovery heavily involves the immune system, Dr. Seo and colleagues began to consider different immune factors that might be impacted by the robotic mechanical stimulation. In this next round of experiments, Dr. Seo again exposed mice with injured muscle to mechanical stimulation. Since there was no difference in the three groups based on the amount of force delivered, they decided to move forward with the group that received 0.3N of force for subsequent studies.
The variable in this next series of experiments was time. After specific time periods, the researchers analyzed the injured muscle tissue and quantified the presence of different types of immune cells. The researchers compared the relative quantities of immune cells at 3, 7, and 14 days in the treatment group of injured mice who received treatment and injured mice who did not receive treatment.
At first, Dr. Seo and her team hypothesized that macrophages would play a role in the observed effects of mechanical stimulation on muscle injury repair, since macrophages are known to play an important role in tissue regeneration (Handschin and Spiegelman, 2008). However, the researchers found the presence of macrophages did not greatly differ over the course of treatment.
To determine whether there might be other types of immune cells involved, the researchers broadly screened the movement of various types of immune cells from the muscle tissue over time. The results of these studies showed that a different type of white blood cell, known as a neutrophil, remarkably decreased after three days of mechanical stimulation compared with injured mice who did not receive treatment.
Neutrophils are one of the most common types of immune cells, comprising 40-70 percent of the total white blood cell count in humans. Since neutrophils are some of the first responders of the immune system, it was thought that they are the first to arrive at an injury and also the first to leave. Previous researchers had hypothesized that if neutrophils stayed too long at the site of injury, they might cause damage by turning against the damaged muscle tissue.
To better understand how neutrophils contributed specifically to muscle regeneration (healing), Dr. Seo and colleagues designed a new experiment. Dr. Seo wanted to see how muscle progenitor cells (MPCs) would grow and then
differentiate
into different types of muscle cells when exposed to different environmental conditions. The control condition was standard cell
growth media
typically used when growing cells in the laboratory. The experimental condition was a specialized media that contained factors released by neutrophils. The purpose of the experiment was to understand how exposure to neutrophils would impact the growth and differentiation of muscle tissue.
After observing cell growth in both of these conditions over time, Dr. Seo and colleagues found that MPC growth increased significantly when exposed to the neutrophil-enriched environment compared with the control environment. This showed that neutrophils do support the growth of MPCs. However, when the researchers looked at cell differentiation, they found the opposite result. MPCs in the neutrophil-enriched environment differentiated significantly less than the control cells. “This data suggests that neutrophils both support and prevent muscle tissue healing depending on the length of exposure,” commented Dr. Seo. In other words, in the first few days after muscle injury, neutrophils are an important factor contributing towards muscle healing. However, if the neutrophils stay at the site of injury too long, they actually prevent the growth of new muscle tissue.
Further testing with robotic mechanical stimulation revealed the primary reason the treatment was so effective for treating muscle injury in mice was because it helped clear neutrophils from the injured site earlier than the body would on its own. Dr. Seo and colleagues confirmed this result using specific antibodies to block neutrophils from entering the injured muscle tissue 1, 2, and 3 days after injury, which is the time frame where the significant reduction of neutrophils were seen. Muscle recovery looked similar in mice who received mechanical stimulation and in mice who received antibodies to block neutrophils (Figure 7).
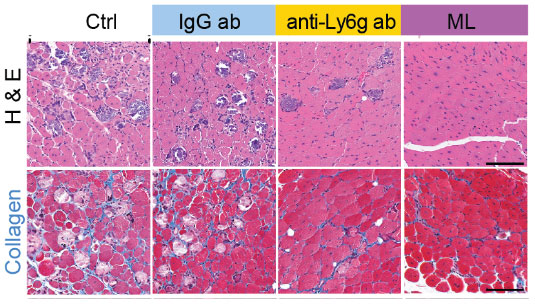
Figure 7. Mechanical loading (ML) and antibodies that block neutrophils from entering the cells (anti-Ly6g ab) help clear neutrophils from muscle tissue when compared to controls (Ctrl and IgG ab). This can be seen in muscle fibers (top row, H & E) and connective tissue (bottom row, Collagen)
[Source: Seo et al. 2021]
This study sheds important light on how massage therapy can help injured muscles recover in a non-invasive way. Dr. Seo and colleagues also identified neutrophils as both a mediator and inhibitor of muscle recovery depending on when and how long they were present at the injured site. The next steps for this research are to conduct similar experiments in larger animal models, such as rabbits and pigs.
Dr. Bo Ri Seo is a research scientist at Takeda Pharmaceuticals. She pursued this research as a Postdoctoral Fellow in the laboratory of Dr. David Mooney. She was trained as a biomedical engineer, and her research focuses on the role of mechanical therapy in muscle regeneration. When not in the laboratory, Dr. Seo enjoys painting, swimming, and traveling. Dr. Seo would like to share one bit of advice for the next generation of scientists: Be persistent but never get too tied up with one hypothesis. Be flexible enough to let the data guide you.
For More Information:
- Seo, B. et al. 2021. “Skeletal muscle regeneration with robotic actuation-mediated clearance of neutrophils.” Science Translational Medicine, 13(614). https://www.science.org/doi/10.1126/scitranslmed.abe8868
- Brownell, L. 2021. “Massage doesn’t just make muscles feel better, it makes them heal faster and stronger.” https://wyss.harvard.edu/news/massage-doesnt-just-make-muscles-feel-better-it-makes-them-heal-faster-and-stronger/
- Peiseler, M. and P. Kubes. 2019. “More friend than foe: the emerging role of neutrophils in tissue repair. J Clin Invest, 129: 2629-2639. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6597202/
- Tidball, J. 2017. “Regulation of muscle growth and regeneration by the immune system.” Nat Rev Immunol 17, 165-178. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5452982/
- Mann, C.J. et al. 2011. “Aberrant repair and fibrosis development in skeletal muscle.” Skeletal Muscle, 1(1): 21. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3156644/
- Schiaffino, S. and C. Reggiani. 2011. “Fiber types in mammalian skeletal muscles.” Physiol Rev 91: 1447-1531 https://journals.physiology.org/doi/full/10.1152/physrev.00031.2010?rfr_dat=cr_pub++0pubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org
- Handschin, C. and B. M. Spiegelman. 2008. “The role of exercise and PGC1alpha in inflammation and chronic disease.” Nature, 454: 463-469. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2587487/
To Learn More:
- Mooney Laboratory. https://mooneylab.seas.harvard.edu/
- Wyss Institute for Biologically Inspired Engineering. https://wyss.harvard.edu/
- Harvard Biodesign Laboratory. https://biodesign.seas.harvard.edu/
- Mayo Clinic. https://www.mayoclinic.org/healthy-lifestyle/stress-management/in-depth/massage/art-20045743
- National Center for Complementary and Integrative Health. https://www.nccih.nih.gov/health/massage-therapy-what-you-need-to-know
Written by Rebecca Kranz with Andrea Gwosdow, PhD at www.gwosdow.com
HOME | ABOUT | ARCHIVES | TEACHERS | LINKS | CONTACT
All content on this site is © Massachusetts
Society for Medical Research or others. Please read our copyright
statement — it is important. |

