Highlights
- Developing diagnostic tools for hard-to-detect cancers can be challenging. Dr. Moses and her team compared the urine of breast cancer patients to those of patients without any cancer. They found biomarkers in urine that were highly predictive of specific types and stages of breast cancer.
- Using similar techniques, Dr. Moses and her team are developing diagnostic urine tests for hard-to-detect cancers, like pancreatic cancer, that could be run using an attachment to a smart phone.
- Moses and her laboratory team are also developing targeted delivery systems to help treat disease once it has been diagnosed. They have developed a targeted drug-delivery system using liposomes for triple negative breast cancer. This drug delivery system is being tested in vivo.
How do doctors find treatments for disease? Before treatment options can even be considered, doctors need a way to diagnose specific diseases. This is why scientists work to develop specific tools to diagnose disease, known as
diagnostics.
Diagnostics are critical for identifying disease early. This is especially important for cancer, which becomes worse over time.
Diagnostic tools already exist for some types of cancer. For example, women over a certain age receive regular
mammograms
to detect breast cancer early, and it is recommended that all adults over a certain age receive routine
colonoscopies
to check for colon cancer. Some cancers are less common and harder to detect, though, and it is impractical to test every adult for every type of cancer. Hard-to-detect cancers include ovarian cancer, pancreatic cancer, and brain cancer. Often by the time patients start having symptoms and this type of cancer is identified, it has already traveled outside the original organ and is much more difficult to treat.
Dr. Marsha Moses is a Professor at Harvard Medical School and Director of the Vascular Biology Program at Boston Children’s Hospital. Dr. Moses and her lab are working to develop diagnostic tools for hard-to-detect cancers. These tools are also used to determine if a given treatment is working, which means the growth of the cancer has stopped or slowed.
Detecting Cancer
Dr. Moses has spent much of her career conducting research to identify proteins in the urine that might indicate disease. Such proteins are known as
biomarkers
because they appear in the urine when a particular type of cancer is present. Dr. Moses has focused on biomarkers in the urine because urine is easy to obtain, completely non-invasive, and pain free.
Dr. Moses and her research team began investigating biomarkers in the urine of cancer patients by developing a
biorepository
of urine samples taken from patients of all ages with all types of cancers. Dr. Moses and her team used a technique called
mass spectrometry
to identify proteins in urine by their mass and electric charge.

Figure 1. Picture of mass spectrometry machine.
[Source: https://www.ucl.ac.uk/chemistry/mass-spectrometry-facility]
Dr. Moses and her colleagues began by testing the urine of breast cancer patients for two proteins associated with breast cancer, matrix metalloproteinases (MMP) and A Disintegrin and Metalloprotease 12 (ADAM12). The levels of these proteins are known to be elevated in patients with some types of breast cancer. Dr. Moses’s laboratory showed that MMP and ADAM12 could also be found in the urine of breast cancer patients.
Next, Dr. Moses and her team compared the urine of breast cancer patients to those of patients without any cancer. The patients without cancer served as controls and were age- and gender-matched to the patients with breast cancer in order to make accurate comparisons between the two groups.
Using this technique, the researchers identified which proteins were expressed in breast cancer patients compared to the matched control patients. The researchers observed that MMP and ADAM12 were found in large quantities in breast cancer patients but not in the matched controls. Based on these results, Dr. Moses and her team concluded that certain MMPs and ADAM12 in the urine were highly predictive of breast cancer.
Using similar techniques, Dr. Moses and her team also identified urine biomarkers for other types of hard-to-detect cancers, like pancreatic cancer. Dr. Moses is currently working to develop diagnostic urine tests that could be run using an attachment to a smart phone. “We don’t imagine that the test would be absolutely definitive,” explained Dr. Moses. “Rather, it will act as a warning sign that there might be something happening with your cancer, so you should see your doctor and get checked out.” Dr. Moses envisions this technology could be used anywhere, even in places without access to health care.
Designing a Precision Drug-Delivery System
In addition to developing diagnostic tools to help find hard-to-detect diseases, Dr. Moses and her laboratory team also work to develop targeted delivery systems to help treat disease once it has been diagnosed. Targeted delivery systems help target the drug, such as
chemotherapy,
to specific cells in the body, like cancer cells.
The drug-delivery system developed by Dr. Moses and her research team uses small droplets called
liposomes.
Liposomes have a single layer of fat cells that can be filled with another substance, such as water or a cancer drug. The outside of the liposome is coated with specific proteins that only recognize the target cells.
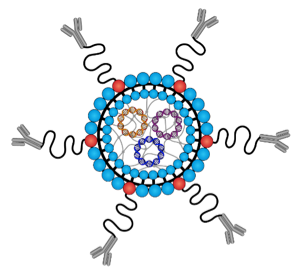
Figure 2. Schematic of a liposome.
[Source: Moses Laboratory]
Dr. Moses and her research team developed this targeted drug-delivery system first for
triple negative breast cancer.
They chose triple negative breast cancer because this type of cancer is highly aggressive, affects African American, Latina, and Caucasian women, and is hard to treat.
The researchers began by identifying all of the
receptors and proteins
on the surface of triple negative breast cancer cells using flow cytometry. They tested many possible binding proteins. To determine which proteins to target on the surface of the breast cancer cells, they used a technique called
atomic force microscopy.
Atomic force microscopy measures how tightly each receptor protein binds with another type of protein, called an
antibody.
The protein that bound tightest was the antibody chosen to coat the liposome to make sure the liposome targeted the cancer cells.
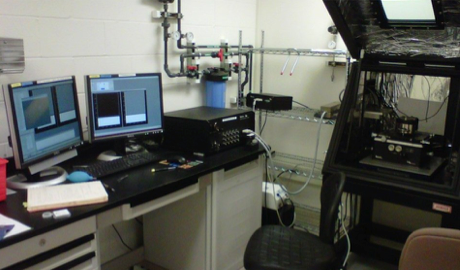
Figure 3. Picture of atomic force microscopy machine.
[Source: Moses Laboratory]
Once a drug-delivery system has been developed, the next step is to test it over and over again. First the system is tested in vitro with tumor cells. If the delivery system passes that test, the researchers test the delivery system in vivo using animals such as mice. Dr. Moses hopes this system will eventually be tested in clinical trials and coupled with her laboratory’s non-invasive biomarkers to develop
“precision medicine”
approaches for cancer and other diseases. This would be a large advance and would provide effective treatment for triple negative breast cancer, a disease for which there are currently few treatment options.
Dr. Marsha Moses is the Julia Dyckman Andrus Professor at Harvard Medical School and the Director of the Vascular Biology Program at Boston Children’s Hospital. She is a biochemist who has pioneered the use of urine biomarkers to diagnose and treat disease. In her spare time, Dr. Moses enjoys developing new research projects and spending time with her family.
For More Information:
- Guo, P. et al. 2018. “Using atomic force microscopy to predict tumor specificity of ICAM1 antibody-directed nanomedicines.” Nano Letters, 18: 2254-2262.
- Guo, P. et al. 2016. “ICAM-1-Targeted, Lcn2 siRNA-encapsulating liposomes are potent anti-angiogenic agents for triple negative breast cancer.” Theranostics, 1: 1-13.
- Pories, SE. et al. 2008. “Urinary metalloproteinases: Noninvase biomarkers for breast cancer risk assessment.” Cancer Epidemiology Biomarkers & Prevention, 17(5): 1034-1037.
To Learn More:
- A Rosy Future. http://www.whatayear.org/01_16.php
- Triple Negative Breast Cancer. https://www.cdc.gov/cancer/breast/triple-negative.htm
- Precision Medicine. https://www.cdc.gov/features/precision-medicine/index.html
- Theranostics. http://theranostics.com.au/what-is-theranostics/
Written by Rebecca Kranz with Andrea Gwosdow, PhD at www.gwosdow.com
HOME | ABOUT | ARCHIVES | TEACHERS | LINKS | CONTACT
All content on this site is © Massachusetts
Society for Medical Research or others. Please read our copyright
statement — it is important. |

