| |
Highlights
- Sleep is important—get more of it for your physical and mental well-being!
- Mental illness changes the sleep-wake cycle and sleep patterns may be used to diagnose mental illness.
- The genes associated with sleep and mental illness overlap and may be responsible for the changes in sleep patterns observed in patients with schizophrenia and bipolar disorder.
Did you know that you spend about a third of your life asleep? This means that the average adolescent has already devoted about 4 to 6 years of life to sleep. "It really is critical!" exclaims Dr. Russell Foster, Professor of Circadian Neuroscience at Oxford University and sleep enthusiast. "There is no activity more important. If you don't snooze, you lose, and you lose big."
What happens while we are sleeping that is so important to our waking hours? How does sleep disruption cause disease? "We can only begin to answer these questions," explains Dr. Foster. Sleep has been disregarded for centuries, even millennia as a nuisance, an annoyance, a chore. It is only in the past few decades that scientists have begun to look seriously at the science of sleep. What they have discovered is only the tip of the iceberg, but even that may be enough to make you jump in bed a few hours earlier tonight.
Sleep and Health
Sleep increases our ability to make good decisions, to be creative and to solve complex problems. But insufficient sleep leads to cognitive impairment including poor judgment and memory, difficulty making decisions and lack of focus and attention. Most of us are familiar with the problems that come from just a few hours of reduced sleep time or disrupted sleep. Drifting off in class, although not recommended, is only a minor example of a much larger problem. Sleep deprivation leads to highway accidents (approximately 100,000 per year in the US) and mistakes at work—potentially deadly mistakes if you happen to be an air traffic controller or doctor, for example.
Sleep disruption is also linked to
obesity.
Studies have shown that people who regularly sleep less than five hours per night have a 50% likelihood of being obese. Why? Sleep deprivation alters levels of hormones, such as
ghrelin,
that are associated with our sense of hunger. Elevated ghrelin levels cause our bodies to crave sugars and starches—the high-calorie, low-nutrient fare of midnight snacks. Over time, this sort of eating behavior can lead to obesity and an increased risk of
cancer,
diabetes,
heart disease
and other illnesses.
In addition, lack of sleep stimulates the release of stress hormones, like
adrenocorticotropic hormone
and
cortisol.
Elevated levels of stress hormones can suppress the
immune system.
This means that chronically tired people are at a higher risk for getting sick and developing infections because the cells normally involved in preventing disease are not working at maximum capacity. Chronic stress is also associated with the development of diabetes, heart disease and many other health conditions.
A Chance Encounter
Dr. Foster studies
circadian rhythms,
also called the "biological clock," that regulate a healthy sleep-wake cycle. Complex interactions between our internal biology and the external environment work together to make us sleepy at night and wake us up the next morning—if the system is functioning normally. In modern life we live indoors much of the time so we are hidden from natural light during the day, and we are exposed to artificial light at night from multiple sources. As a result it has become even easier for the biological clock to get confused or disrupted.
For many years, Dr. Foster focused his research on how the biological clock interprets light signals. "I was always interested in circadian rhythms," he recalls. "But I had never really honed in on the sleep part of the sleep-wake cycle." That is, until a chance encounter in the elevator.
On a day like any other at the university, Dr. Foster got on the elevator with a colleague in
psychiatry.
The psychiatrist was upset that a patient had missed an appointment and made a comment that people with
mental illness
sleep too much. "I had no training in psychiatry," recalls Dr. Foster. "But this observation struck me as odd." Out of mere curiosity, he began to look into the association between sleep and mental illness. He started collaborating with colleagues in psychiatry, psychology and other fields. "This was driven by pure curiosity," Dr. Foster recalls. "I had no idea where it might take me."
Sleep and Mental Illness
It turns out that Dr. Foster's intuition was correct. Psychiatric patients often experience frequent sleep disruption. "It is something about mental illness itself that completely changes the sleep-wake cycle in some of these patients," he explains. The relationship is actually more complex than that, because sleep disruption and mental illness seem to share overlapping neural networks in the brain so changes in these pathways that lead to mental illness will also disrupt sleep.
The sleep disruption makes the mental illness worse, while the mental illness makes the sleep disruption worse.
In collaboration with his colleague, Dr. Katharina Wulff, Dr. Foster was able to study long-term sleep-wake cycles in patients with
schizophrenia.
Schizophrenia is a chronic, often severe and debilitating, psychiatric disorder characterized by paranoid thoughts, hallucinations and a loss of connection between thoughts, emotions and reality. A common symptom of patients with schizophrenia is irregular sleeping patterns.
Traditionally sleep studies had to be conducted in a clinical setting, with the patient staying overnight in the hospital, hooked up to lots of machines. This is not possible with people with schizophrenia. Instead, Dr. Foster and his colleagues developed a method to gather comparable data from the home environment. They used a wristwatch with movement and light detectors that sensed when the wearer was asleep or awake. The data gathered from the watches in addition to patient sleep diaries were used to estimate sleep-wake cycles. What the researchers demonstrated with these human studies provided experimental support for a large body of anecdotal evidence. "The data were remarkable," comments Dr. Foster. "The sleep-wake cycles of patients with schizophrenia were absolutely smashed."
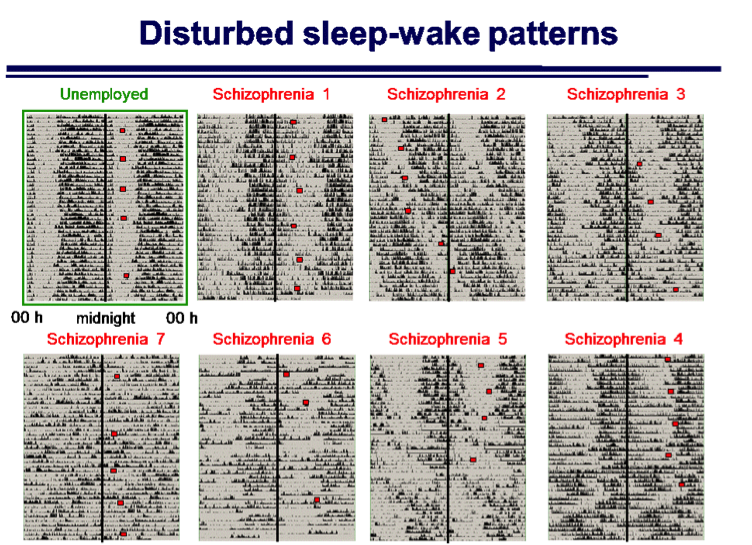
Examples of the variability in sleep/wake patterns from seven subjects with a diagnosis of schizophrenia compared to an unemployed "control" subject. Each line shows 48h of activity and the vertical line in each record indicates midnight. The unemployed subject shows a stable sleep/wake activity profile, and that the peak in the hormone melatonin (red square) occurs at the same time over the study period. By comparison the sleep/wake of schizophrenia patients are all highly irregular, and in many cases most activity occurs during the night.
"We have shown that sleep disruption and schizophrenia share common pathways. The genes associated with schizophrenia and the genes associated with sleep disorders actually overlap."
In order to understand the causes of such extreme alterations in the sleep-wake cycles of patients with schizophrenia, Dr. Foster began working with mouse models. He turned first to the gene for synaptosomal-associated protein 25kDa, (SNAP-25), which had previously been associated with schizophrenia in humans. To see if this protein was also involved in sleep, Dr. Foster and his team of researchers studied mice with a mutant form of the SNAP-25 gene and compared their sleep-wake cycles to control mice with a normal SNAP-25 gene. The sleep-wake cycle measurements were made using sensors that detected movement in mouse cages, much like the wrist-watch sensors of the schizophrenic patients in the previous study.
The researchers observed that mice with the mutant SNAP-25 gene associated with schizophrenia in humans had severe sleep disruption. Follow-up experiments with other schizophrenia-associated genes achieved similar results. "We have gone far beyond a mere association between sleep disruption and mental health," explains Dr. Foster. "We have shown that sleep disruption and schizophrenia share common pathways. The genes associated with schizophrenia and the genes associated with sleep disorders actually overlap."
These findings are already revolutionizing how scientists approach the diagnosis and treatment of mental illness. In a separate study, Dr. Foster, working with Dr. Guy Goodwin at Oxford, compared the sleep habits of adolescents at high and low risk for developing
bipolar disorder.
Bipolar disorder is a psychiatric disorder that usually appears in late adolescence or early adulthood. It is characterized by large swings in mood and energy ranging from severe depression to extreme highs. Patients with bipolar disorder often report sleep disruption.
The researchers in this study of subjects who were at risk of developing bipolar disorder used questionnaires and family interviews to gather information about daily routines and habits including sleep patterns. They found that sleep abnormalities appear prior to the symptoms of mental illness. This is a novel finding that suggests that sleep abnormalities could be used as an early diagnostic tool for those at risk of developing bipolar disorder and other mental illnesses. Early diagnosis can lead to early intervention and improved outcomes for patients. "And it's based on sleep," remarks Dr. Foster. "It is so simple and so profound."
Separately, Dr. Foster's colleague, psychiatrist Dr. Dan Freeman, showed that it was possible to reduce delusional paranoia in patients with schizophrenia by fifty percent using behavioral therapy to partially stabilize sleep patterns. "By targeting just the sleep systems, Dr. Freeman reduced one of the most prominent complaints of patients with schizophrenia," remarks Dr. Foster. "That's amazing."
Encouraged by these initial studies in both animals and humans, Dr. Foster and colleagues established the Sleep and Circadian Neuroscience Institute to bring together researchers and clinicians to understand the mechanisms of sleep regulation and sleep disruption. The scientists are involved in a variety of research projects including mental illness and sleep patterns in adolescents and the aged.
"By targeting just the sleep systems, Dr. Freeman reduced one of the most prominent complaints of patients with schizophrenia," remarks Dr. Foster. "That's amazing."
Possible Treatments
Another important part of Dr. Foster's work is the development of new therapies for mental illness based on these research findings. To begin, he is drawing on the 6,500 drugs already approved by the U.S. Food and Drug Administration (FDA). Most drugs have at least four potential therapeutic purposes but are only approved for one or two by the FDA. In addition, a large number of drugs have sleep-related side effects that alter the sleep-wake cycle. "Since these drugs have been shown to have minimal health risks, this is a good place to start," remarks Dr. Foster.
In order to begin testing these drugs for their influence on the sleep-wake cycle,
Dr. Foster and colleagues first developed an assay system to easily identify drug effects.
So far Dr. Foster and his team have tested over 2,000 drugs and identified 16 that have major effects on the biological clock of these experimental cells. These researchers hope that in the coming years they will identify drugs that can directly target the sleep-wake cycle and improve outcomes for patients with mental illness and other illnesses where the sleep/wake cycle is disrupted.
Sleep and Training Doctors
Sleep abnormalities occur before symptoms of mental illness. Sleep-wake cycles can be used for early diagnosis of mental illness. Early diagnosis can lead to early treatment and improved outcomes for people.
Another important goal of the Sleep and Circadian Neuroscience Institute is education. "In five years, a practicing clinician may receive two or three lectures about sleep," explains Dr. Foster. "This is not nearly enough." Led by Dr. Colin Espie, the Institute has launched a fully online master's degree in sleep medicine to train clinicians and other health-care workers in helping patients with sleep problems and identifying early warning signs of mental illness based on abnormal sleep patterns.
Sleep and Teenagers
Dr. Foster is a strong advocate of sleep for all, particularly teenagers. "For ultimate cognitive performance, teenagers need around nine hours of sleep per night," explains Dr. Foster. "Many teens get only five or six hours of sleep on a school night. That is not nearly enough!" Teenagers are biologically predisposed to go to bed later and wake up later, probably due to changes in sex hormones during puberty. In addition, computers, video games, and social media have worsened the teenage tendency to stay up late. "My biggest advice for teenagers is to get more sleep," concludes Dr. Foster. "For your physical and mental well-being, it's one of the best—and simplest—things that you can do."
Dr. Russell Foster is Professor of Circadian Neuroscience and the Head of the Department of Ophthalmology at The University of Oxford in England. He is also the Director of the Sleep and Circadian Neuroscience Institute. His research interests include the mechanisms that regulate the biological clock and disease states that arise from its disruption. Dr. Foster's most recent work focuses on the connections between sleep and mental illness. When not in the laboratory, Dr. Foster enjoys swimming, theater, opera and spending time with friends and family. In 2015 he was made a Commander of the Order of the British Empire (CBE) by Prince William for his services to science.
For More Information:
- Tam S.K., D. Pritchett, L.A. Brown et al. 2015. "Sleep and circadian rhythm disruption and recognition memory in schizophrenia." Methods in Enzymology 552:325-349.
- Jagannath, A., S. Peirson and R. Foster. 2013. "Sleep and circadian rhythm disruption in neuropsychiatric illness." Current Opinion in Neurobiology, 23: 888-94.
- Freeman D., H. Startup and E. Myers et al. 2013. "The effects of using cognitive behavioral therapy to improve sleep for patients with delusions and hallucinations (the BEST study): study protocol for a randomized control trial." Trials, 14:214.
- Wulff, K., Dijk D.J., B. Middleton et al. 2012. "Sleep and circadian rhythm disruption in schizophrenia." British Journal of Psychiatry, 200: 308-16.
- Oliver P.L., Sobczyk M.V., E.S. Maywood et al. 2012. "Disrupted circadian rhythms in a mouse model of schizophrenia." Current Biology 22:314-319.
To Learn More:
Circadian Rhythms
- Foster R.G. and I. Kreitzman. 2014. "The rhythms of life: what your body clock means to you!" Experimental Physiology 99:599-606.
- Fisher S.P., R.G. Foster and S.N. Pierson. 2013. "The circadian control of sleep." Handbook of Experimental Pharmacology 217:157-183.
Sleep and Mental Health
- Sleep and Circadian Neuroscience Institute. http://www.ndcn.ox.ac.uk/research/sleep-circadian-neuroscience-institute
- "Why do we sleep?" TED talk by Russell Foster. http://www.ted.com/talks/russell_foster_why_do_we_sleep?language=en
Sleep and Sleep Disorders
- National Sleep Foundation. http://sleepfoundation.org/
- National Institute of Neurological Disorders and Stroke. http://www.ninds.nih.gov/disorders/brain_basics/understanding_sleep.htm
- Centers for Disease Control and Prevention. http://www.cdc.gov/sleep/index.html
Schizophrenia
- National Institute of Mental Health. http://www.nimh.nih.gov/health/topics/schizophrenia/index.shtml
- National Alliance on Mental Illness. https://www.nami.org/Learn-More/Mental-Health-Conditions/Schizophrenia
Bipolar Disorder
- National Institute of Mental Health. http://www.nimh.nih.gov/health/topics/bipolar-disorder/index.shtml
- National Alliance on Mental Illness. http://www2.nami.org/Content/NavigationMenu/Mental_Illnesses/Bipolar1/Home_-_What_is_Bipolar_Disorder_.htm
Written by Rebecca Kranz with Andrea Gwosdow, PhD at www.gwosdow.com
HOME | ABOUT | ARCHIVES | TEACHERS | LINKS | CONTACT
All content on this site is © Massachusetts
Society for Medical Research or others. Please read our copyright
statement — it is important. |
|
|

Dr. Russell Foster

Dr. Foster and his research team.
TOP ROW: Tom Watson, Aarti Jagannath, Violetta Pilorz, Sibah Hassan, Russell Foster, Vladyslav Vyazovskiy, Laurence Brown
MIDDLE ROW: Carina Pothecary, Jovi Wong, Eleanor Waite, Jan Cosgrave, Ross Purple, Kate Porcheret, Rukhsana Safa
BOTTOM ROW: Jessica Rodgers, Stuart Peirson, Simona di Pretoro, Sridhar Vasudevan

Medal of the Most Excellent Order of the British Empire
Well-known people who struggled with schizophrenia
Zelda Sayre, shown here with her future husband F. Scott Fitzgerald, had schizophrenia.
John Nash, a Nobel laureate and subject of the movie A Beautiful Mind, had schizophrenia.
Mary Todd Lincoln, wife of President Abraham Lincoln, had schizophrenia.
External Links
TED - Russell Foster: Why do we sleep?
TED - What's the connection between sleep and mental health? A Q&A with circadian neuroscientist Russell Foster
The Financialist - You Snooze, You Lose? Wrong. Russell Foster on the Science of Sleep
Wired - Russell Foster on how sleep science explains eye disease and mental health
NPR - TED Radio Hour - Why Do We Need Sleep?
 Russell Foster: Why do we sleep?
Russell Foster: Why do we sleep?
 Cheltenham Science Festival - rhythm of life - lecture by Prof. Russell Foster.
Cheltenham Science Festival - rhythm of life - lecture by Prof. Russell Foster.
Sign Up for our Monthly Announcement!
...or  subscribe to all of our stories! subscribe to all of our stories!

What A Year! is a project of the Massachusetts
Society for Medical Research.
|
|

