| |
How much air do you breathe? The average adult inhales about seven liters per minute, which is about
11,000 liters of air per day.
It would fill a cube about 7'4" on each side.
That's a lot of air, and also a lot of potentially harmful agents like bacteria and viruses. As one of the only organs in your body in direct contact with the outside world, the lungs are equipped with specific immune mechanisms to prevent disease and keep you healthy. Inevitably, though, some clever organisms are able to overcome these immune mechanisms, causing some of the most widespread and fatal infections like tuberculosis and influenza.
This month, we'll take a tour of healthy lungs, and then lungs infected with tuberculosis and influenza. We'll show you the latest research into pulmonary immune function conducted by Dr. Maziar Divangahi and a team of researchers at McGill University in Canada. Finally, we'll show you some possibilities in the near and not-so-near future for keeping our lungs-and ourselves-healthy and disease-free.
Healthy Lungs
Healthy lungs are perhaps the best-known part of the
respiratory system,
the system responsible for providing cells with oxygen and removing carbon dioxide. Other parts of the respiratory system include the mouth (or oral cavity), nose, and the
trachea,
or windpipe. In fact, the tube connecting the nose and mouth to the lungs is a series of tubes known collectively as the
respiratory tract.
The
upper respiratory tract
refers to the air passages leading from the nasal and oral passageway to the
pharynx
and
larynx.
The pharynx connects to the
lower respiratory tract,
including the trachea and
bronchioles.
The larynx includes the
vocal cords
that allow for speech and sound.
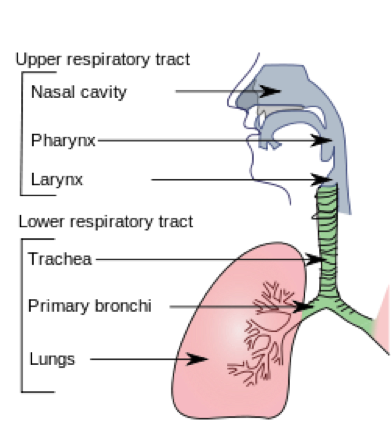
Fig. 1 - Schematic of the upper and lower respiratory tracts.
http://en.wikipedia.org/wiki/Respiratory_tract This is a public domain work.
Air entering the body through the nose and mouth flows through the nasal and oral passageways to the pharynx, trachea and finally into the bronchial tubes that connect the trachea to the lungs. The primary bronchi branch into the right and left lung, and they continue branching into secondary and tertiary bronchi and then smaller
bronchioles
before arriving at the
alveoli,
grape-like sacs that are the site of
gas exchange
in the lungs. On average,
the human lung contains around over 400 million alveoli.
It is here that new oxygen enters the blood stream and carbon dioxide leaves the body, going back through the bronchioles, tertiary, secondary and primary bronchi, up the trachea, pharynx (and larynx, if you're speaking), and finally out the nose and mouth and back into the environment.
Fig. 2 - This short video gives a 3-D demonstration of how breathing works.
http://www.youtube.com/watch?v=hp-gCvW8PRY#t=26
Defense Mechanisms to Prevent and Fight Infection
Since the lungs come in direct contact with the outer environment, the respiratory tract has defense mechanisms to prevent and fight infection. These mechanisms can be categorized into three levels, based on their proximity to the incoming air.
- The first level of defense includes the small hairs, known as
cilia,
which line the nose, nasal passageway, and respiratory tract. The respiratory tract also secretes mucus that traps foreign agents and sends them back towards the pharynx to be swallowed. Coughing is one quick way to remove foreign agents trapped in mucus.
- For
pathogens
that happen to get through the cilia and mucus, proteins in the lining of the respiratory tract form a second line of defense. These proteins are part of the
immune system
and destroy any foreign agents they detect. Often times when we feel sick, we are actually feeling the effects of the immune system fighting pathogens that have entered the airways. In the case of the common cold, the pathogens are caught by the first or second line of defense mechanisms and the infection is quickly resolved.
- Severe infections result when pathogens actually make it into the lungs. In these cases, a final defense mechanism is activated. In healthy lungs, specialized immune cells known as
macrophages
engulf and remove particles that happen to reach the lower airway. When confronted with a pathogen, however, these macrophages trigger an initial inflammatory response that brings more immune cells to the site of infection. As we will see, this inflammatory response can be productive in fighting off infection, but it can also be detrimental to the person's health-and sometimes fatal.
Fig. 3 - Here is how the cilia and mucus work together to help fight infection.
https://www.youtube.com/watch?v=NSXbb5KZl_I
Bacteria or Virus?
This month we will explore two infections of the lungs:
tuberculosis
and
influenza.
These infections differ in one very important respect: tuberculosis is caused by the
bacterium
(Mycobacterium tuberculosis,
to be specific); influenza is caused by a class of
viruses
that include the
seasonal flu
and
pandemic flus
such as the
avian (bird) flu
in 2004 and the
swine (pig) flu
in 2009-2010. The type of microorganism determines how it interacts with our immune system, how the disease progresses, and ultimately how the infection can be treated and prevented.
So what's the difference between a bacteria and a virus? Most basically, bacteria are considered living organisms and viruses are not.
So what's the difference between a bacteria and a virus? Most basically, bacteria are considered living organisms and viruses are not. Bacterial cells have both a
cell membrane
and a
cell wall,
and genetic material floats freely inside; they reproduce through a type of
asexual reproduction
within the
host organism.
Importantly, not all bacteria cause bacterial infections. In fact, humans depend on untold numbers of bacteria to live.
Viruses, on the other hand, are never beneficial. They are not considered living organisms. They consist of genetic material surrounded by a protein coating (not a cell wall) and they cannot reproduce. Instead, viruses invade host cells and exploit the reproduction processes of the host cell. When the host cell dies (often caused by the virus), the viral genetic material is then released to infect other host cells. Viruses cannot be cured. They can only be prevented by vaccines, or in some cases antiviral medications can slow (but not stop) viral reproduction. Bacterial infections, on the other hand, can often be treated with
antibiotics.
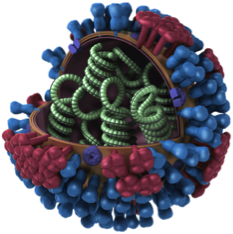
Fig. 4 - Generic image of an influenza virus with part of the outer wall sliced away.
http://www.cdc.gov/flu/images.htm This is a public domain work.
Now let's explore some differences between bacteria and viruses in depth with two examples: the influenza virus and the tuberculosis bacteria.
Influenza
Influenza is a class of infectious viruses that can cause symptoms ranging from mild fever to death. Since viruses combine and interact with host genetic material, new, more
virulent
strains
of the virus have emerged in recent years. Perhaps you are most familiar with the seasonal flu, caused by several strains of the influenza virus. Seasonal flu symptoms are distinct from the common cold and can include fever, chills, body aches and fatigue. The seasonal flu virus can be prevented in most cases by the flu vaccine. This vaccine provides protection against the most common strains of the flu virus. It is still possible to catch the flu, since it is impossible to vaccinate against every strain of the virus, but people who receive the vaccine are much less likely to develop the flu, and if they do, symptoms are usually less extreme. Once you have the virus, though, it cannot be treated by any known remedy. Medications such as aspirin (ibuprofen) can help alleviate symptoms, but the flu just has to run its course.
Flu seasons are unpredictable, and anywhere from 5% to 20% of the population in the United States may contract the infection in any given year,
according to the Centers for Disease Control and Prevention.
More than 200,000 people are hospitalized each year for flu-related complications, and some number of them will die from the disease. Most hospitalizations and fatalities occur in the very young and very old.
Not all of these hospitalizations and deaths are caused by the flu virus itself. Instead, flu complications and deaths are sometimes the result of an ineffective immune response. To understand why, let's follow the influenza virus as it infects its host human.
The flu virus entering the human body is too small to be trapped by the cilia and mucus of the upper respiratory tract and often makes it past the immune cells of the respiratory tract wall. As the virus enters the alveolar sacs in the lungs, it triggers an initial immune response by the macrophages, which activates other immune cells to secrete chemicals, known as
cytokines,
to help fight the infection. In healthy adults, this battle between the immune system and the virus lasts 7-10 days, after which the virus is successfully defeated and symptoms clear up.
In infants and children the immune response is so strong that it overwhelms the growing hosts. In these cases, the smallest casualties of the influenza virus are killed not by the viral infection, but by their own immune response.
But in the elderly and other adults with weaker immune systems, the immune system is sometimes not strong enough to fend off infection. It is these cases that result in hospitalization and, sometimes death. In infants and children, on the other hand, the immune response is so strong that it overwhelms the growing hosts. In these cases, the smallest casualties of the influenza virus are killed not by the viral infection, but by their own immune response. Finally, in the case of pandemic flu viruses like avian and swine flu, the body has never seen the virus before, so in some people the immune system will over-react, launching a larger-than-needed operation to bring the virus down. In these cases, sometimes even otherwise healthy adults, in addition to children and the elderly, can succumb, not to the influenza virus, but to the consequences of their own immune systems.
In cases of flu complications, the resulting hospitalizations and deaths are caused by an immune response that is out of proportion-either too big or too small. In his research into the influenza virus, Dr. Divangahi sought to understand the immune response in more detail in the hopes of reducing the number of viral infections, and resulting deaths.
Dr. Divangahi and his colleagues were interested in the role of anti-inflammatory drugs like aspirin and other
non-steroidal anti-inflammatory drugs
(NSAIDS-other examples include Tylenol and Advil), which are commonly used to treat flu symptoms. These medications target signaling molecules, called
eicosanoids,
that are responsible for regulating the immune response. In particular, NSAIDS inhibit a class of eicosanoids called
prostaglandins,
which usually stimulate an immune response. By preventing the normal function of prostaglandins, these over-the-counter medications reduce inflammation and other symptoms that result from normal immune function.
There are many types of prostaglandins, however, and Dr. Divangahi and his colleagues wanted more specific information about which prostaglandins were targeted by the NSAIDS. To determine which prostaglandins were most important in the anti-inflammatory response, Dr. Divangahi and his colleagues developed mice models, called
"knock out" mice,
which lacked genetic information specific to a certain prostaglandin. They then introduced the influenza virus into a group of "knock-out" mice without the specific gene and compared the infection outcomes of the experimental mice with a group of mice with the full genetic information (control mice). Over several years, the researchers performed a series of these experiments with a variety of prostaglandins to determine the effects of each one. From the results, the researchers identified a single prostaglandin, called prostaglandin E2, or PGE-2 for short, which was most responsible for the inflammatory response associated with the influenza virus. In fact, the researchers showed that mice that genetically lacked PGE-2 were able to survive an otherwise lethal dose of the influenza virus.
The next step was to determine why the lack of PGE-2 allows these mice to survive influenza infection. Put another way, the researchers wanted to know how the presence of PGE-2 in both mice and humans contributed to the infection process. This knowledge, in turn, could help lead to potential treatments for the disease.
In order to understand the significance of PGE-2, researchers had to take a broader view of the inflammatory process beginning with the production of PGE-2. As we have already described, when macrophages detect a foreign agent such as the influenza virus, they send out signaling molecules called cytokines to call for more help at the infection site. PGE-2 is one of these cytokines. Its presence inhibits the production of its target molecule, an immune protein called Type 1 Inteferon. Type 1 Interferon, abbreviated as Type 1-IFN, has been previously identified as an anti-viral agent, making it an important immune molecule for preventing viral infections.
"It is clear from these experiments that the influenza virus is intentionally stimulating the production of PGE-2 to create a better environment for its replication," explains Dr. Divangahi. The researchers do not yet know the mechanism that allows the virus to stimulate PGE-2 production. Dr. Divangahi suspects that one or several proteins within the virus are involved, and current experiments are underway to determine exactly which ones. "At any rate, this is a really exciting discovery," remarks Dr. Divangahi. Based on their results, the researchers propose that inhibiting PGE-2 during influenza infection could help treat the disease.
Such treatments, however, are still years away.
What is bad for a virus (and a potential treatment for influenza infection) could actually be good for bacteria.
The development of anti-viral remedies targeting PGE-2 is further complicated by the fact that what is bad for a virus (and a potential treatment for influenza infection) could actually be good for bacteria. To understand why, let's now turn from viral lung infections to bacterial ones.
Tuberculosis
Tuberculosis (TB) is a bacterial infection usually affecting the lungs caused by the bacterium Mycobacterium tuberculosis, or Mtb for short. In 2012, the World Health Organization estimates that 8.6 million people developed the disease and about
one-third of those who contracted the disease died from it
(about 1.3 million people). Although TB is not a major health concern in North America and Europe, it is a major problem in India, China, and many African countries. TB is also extremely
pathogenic,
meaning it can spread easily from one person to another through the airways: all it takes is just a few bacteria exhaled by an infected person coughing or sneezing and subsequently inhaled by an uninfected person to cause a major infection.
TB bacteria are generally able to proceed uninhibited through the cilia and mucus of the airways first line of defense, and then the secondary defense of the immune cells in the respiratory tract. The macrophages-the third and final defense mechanism to protect the lungs-are activated to prevent infection, like they are in the case of influenza. But the Tuberculosis bacteria actually target the macrophages for infection, where they settle and reproduce. "In the case of TB, the macrophages become bacterial heaven," explains Dr. Divangahi. "TB has taken over the very cells that are supposed to destroy them."
Many people infected with Mtb go years or even decades without symptoms. Some may never develop acute infection at all. Whether or not acute infection develops, though, anyone with the Mtb bacteria can spread the disease. This is what makes TB so powerful-you can spread it without knowing. This is one reason TB tests have become routine procedure for those spending time in other countries where the disease is prevalent, and also for anyone working in health-related fields.
Acute tuberculosis infection develops when the bacteria that initially infected the macrophages kill the host cells and break free. If the macrophages were to die a healthy death, the cell membrane would remain intact, trapping and killing the bacteria inside and alerting healthy macrophages to their presence. This form of cell death is called
apoptosis.
In the case of TB, however, the infection causes the cells to die by dissolving the cell membrane, a process known as
necrosis,
which allows the bacteria to be released and free to infect additional macrophages.
Whether infected macrophages die through apoptosis (cell membrane intact) or necrosis (cell membrane dissolved) is a finely tuned process regulated, in part, by prostaglandins. In fact, PGE-2 plays an important role in the development of TB just as it does in influenza. Dr. Divangahi and his team have found that PGE-2 stimulates cell death by apoptosis, thereby acting to prevent bacterial infection. The TB bacteria, however, suppress PGE-2 by stimulating another class of eicosanoids that counteract PGE-2, which are called Lipoxin A4 or LXA-4.
"We see in the case of TB that PGE-2 plays a positive role in fighting bacterial infection," explained Dr. Divangahi. Recall, however, that this is the opposite of what PGE-2 does in the case of viral infection. Whereas PGE-2 works with the immune system against bacterial infection, it works against the immune system to promote disease in the case of viral infections. "This makes the development of treatments for either tuberculosis or influenza based on PGE-2 quite complicated," remarked Dr. Divangahi.
Super Infections
The results from Dr. Divangahi's work also help explain a commonly observed pattern that occurs when a patient contracts a bacterial infection on top of a viral infection. This double infection is known as a
"super" infection.
Why does this happen? Dr. Divangahi explains: "When you contract a viral infection, your body wants to rapidly increase the levels of the anti-viral agent Type 1-IFN." It does this by inhibiting the production of PGE-2. As we have just seen, though, PGE-2 is an important anti-bacterial agent. "In the process of fighting off viral infection, the body actually makes itself more susceptible to bacterial infection." The same is true in the other direction. When you first contract a bacterial infection, the body produces increased amounts of the anti-bacterial agent PGE-2. In doing so, it significantly decreases the amount of anti-viral Type 1-IFN, leaving the body more vulnerable to viral infection. In both cases, a super infection can result.
Bench to Bedside
Dr. Divangahi's research has shown the importance of PGE-2 in determining the course of both bacterial and viral infections. Treatments based on PGE-2, however, are complicated by the antagonistic roles PGE-2 plays in the course of bacterial versus viral infections. "Clearly PGE-2 plays an important role in the development of these infections, but it may not be the best target for treatment," Dr. Divangahi cautioned. In the case of tuberculosis, Dr. Divangahi believes we need to find a way to prevent initial infection. One possibility could be a system that allows the body to increase the production of macrophages to prevent infection in areas with high disease prevalence. Ongoing research in Dr. Divangahi's laboratory is focusing on the role of
mitochondria,
and their involvement in cell death pathways.
"We still have a long way to go towards understanding how the immune system works to fight and prevent infection," Dr. Divangahi commented. "That's what makes my job so exciting."
Dr. Divangahi is a
pulmonary immunologist
whose research focuses on the mechanisms by which the pulmonary immune system fights and prevents infection. He is Assistant Professor of Medicine at McGill University, and Research Director of the Meakins-Christie Laboratories. He is also a member of the McGill International TB Centre. Dr. Divangahi is a committed athlete and enjoys running, biking, hiking and swimming, among other outdoor activities outside the laboratory. He also spends as much time as possible with his family.
To Learn More:
- Jaworska, J. et al. 2014. "NLRX1 prevents mitochondrial induced apoptosis and enhances macrophage antiviral immunity by interacting with influenza virus PB1-F2 protein." Proceedings of the National Academy of Sciences, E2119.
- Coulombe, F. et al. 2014. "Targeted prostaglandin E2 inhibition enhances antiviral immunity through induction of Type 1 Interferon and apoptosis in macrophages." Immunity, 40(4): 554-68.
- Full, F. and M. Gack. 2014. "Prostaglandin E2: the Villain in the Host Response to Influenza Virus." Immunity, 40(4): 453-4.
- Divangahi, M. et al. 2013. "Dying to Live: How the Death Modality of the Infected Macrophage Modulates Immunity to Tuberculosis." The New Paradigm of Immunity to Tuberculosis, Advances I Experimental Medicine and Biology. http://www-ncbi-nlm-nih-gov.ezp-prod1.hul.harvard.edu/pubmed/23468106
For More Information:
- Dr. Divangahi's homepage: http://meakins.mcgill.ca/divangahi.php
Tuberculosis
- World Health Organization. http://www.who.int/topics/tuberculosis/en
- Centers for Disease Control and Prevention. http://www.cdc.gov/tb
- National Health Service (UK). http://www.nhs.uk/conditions/Tuberculosis/Pages/Introduction.aspx
Influenza
- World Health Organization. http://www.who.int/topics/influenza/en
- Centers for Disease Control and Prevention. http://www.cdc.gov/flu
- Influenza Research Database. http://www.fludhb.org/brc/home.spg?decorator=influenza
Written by Rebecca Kranz with Andrea Gwosdow, PhD at www.gwosdow.com
HOME | ABOUT | ARCHIVES | TEACHERS | LINKS | CONTACT
All content on this site is © Massachusetts
Society for Medical Research or others. Please read our copyright
statement — it is important. |
|
|

Dr. Divangahi's Lab Team
Sign Up for our Monthly Announcement!
...or  subscribe to all of our stories! subscribe to all of our stories!

What A Year! is a project of the Massachusetts
Society for Medical Research.
|
|

