Humans must eat to survive. Your body reminds you of this several times per day through a cascade of signals we interpret as hunger. What people eat to alleviate their hunger varies dramatically across the globe. Nevertheless, any healthy diet must provide the body with sufficient energy and the nutrients that it cannot produce on its own. These nutrients are the building blocks that enable our bodies to remain happy and healthy. They are so critical that deficiency in particular nutrients can result in disease. The specific ways that diet influences the development of disease is the focus of an emerging scientific field known as
nutritional immunology.
This month, we highlight the research of the eminent nutritional immunologist, Dr. Philip Calder from the University of Southampton, England. In particular, we will focus on Dr. Calder’s research into the effects of
fatty acids
on the development of
allergies
and
asthma.
Diet and the Immune System
Let’s begin with the
immune system
and how it functions. Unlike other systems in the body that are centered around a specific organ like the heart or the lungs, the immune system does not have a single locus. Immune cells originate in the
bone marrow
and then differentiate into a variety of cell types that reside in certain organs or that circulate throughout the bloodstream. These cells identify potentially harmful substances in the body and work together to neutralize them. When working properly, the immune system protects the body from external threats such as bacteria and viruses.
A poor diet can reduce the ability of the immune system to keep you healthy and disease-free.
There are several ways that our diet can influence the proper functioning of the immune system. Most broadly, the immune system requires energy to function and to continually produce new immune cells. In addition, immune cells may require specific nutrients in the diet to induce or speed up a chemical reaction. As a result, nutrients can influence the balance between different types of immune cells; a balance necessary for proper immune function. A poor diet can reduce the ability of the immune system to keep you healthy and disease-free. In contrast, a healthy, balanced diet can promote immune function to keep you healthy and strong.
In his investigations into the correlation between diet and disease, Dr. Calder focuses on molecules called fatty acids. These are the components of
large fat
molecules like
saturated
and
unsaturated fat.
The words “fat” and “fatty acid” are often used interchangeably. All you need to remember is that one molecule of fat contains several (typically three) fatty acids. The terms “saturated” and “unsaturated” refer to the number of hydrogen atoms attached to the carbon chain. Although this may seem like a small detail, the number of carbon-hydrogen bonds affects the shape and therefore the function of the molecules.
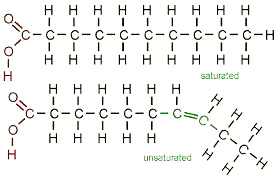
Saturated and unsaturated fats
There are three primary types of fatty acids:
saturated fatty acids,
found primarily in animal products;
monounsaturated fatty acids
found in avocados, olives, and nuts; and
polyunsaturated fatty acids,
found in vegetable oils and fish. In particular, Dr. Calder focuses on two types of polyunsaturated fatty acids: omega-6, found in vegetable oils; and omega-3, found in fish and fish oils. There are primarily two types of omega-3 fatty acids in fish: docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA)
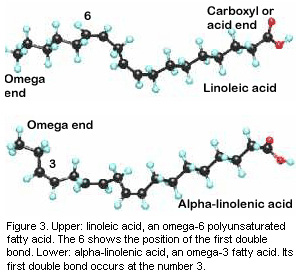
Omega-3 and omega-6 fatty acids
An appropriate balance of different fatty acids helps regulate the
inflammatory response.
- Saturated fatty acids and omega-6 fatty acids both increase the inflammatory response because, as they break down, their component parts become pro-inflammatory signals.
- Monounsaturated fatty acids and omega-3 fatty acids, on the other hand, interfere with the inflammatory response and act as anti-inflammatory agents.
Diet and Disease
Researchers have identified particular conditions in which the correlation between diet and disease is high. One such condition is food allergies. Allergies are the result of improper immune function. In a healthy person, food should not trigger an active immune response. In some people, though, the immune system mistakenly identifies a food item, such as peanuts or shellfish, as an external threat. The consistent active immune response to an ingested food item is known as a food allergy. Many children develop food allergies early in life but grow out of them over time. Even if a child no longer exhibits signs of a food allergy, though, the child remains at a higher risk for developing asthma, a life-long condition characterized by inflammation of the lungs and narrowing of the airways.
It is possible that the immune system may become compromised by certain components of our modern diet.
Why do food allergies develop? Researchers have several theories, although the exact process remains unknown. First, an immune system that is not sufficiently exposed to bacteria and viruses early in life may come to recognize harmless substances as potentially damaging. Many researchers believe that our modern environment is too clean and therefore prevents children from developing appropriate immune defenses. Second, it is possible that the immune system may become compromised by certain components of our modern diet. Dr. Calder believes that this second factor in particular may explain the rising rate of allergies and asthma that researchers have observed in the past fifty years.

Salmon are high in omega-3 fatty acids
Specifically, Dr. Calder has focused his attention on the types of fats we eat and how they have changed over time. He notes that people in the United States eat less omega-3 fatty acids like those found in oily fish (anchovies, trout, tuna, mackerel, herring, salmon, and sardines) and more omega-6 fatty acids found in many processed foods. Omega-6 fatty acids have been linked to an increased predisposition to allergies.
A Dietary Intervention
Dr. Calder wondered whether allergies might result from an imbalance between omega-3 and omega-6 fatty acids in the body. To test his hypothesis, he created a dietary intervention for healthy pregnant women who were half way through their pregnancy. In a total of 123 pregnant women, half (62 women) were given salmon (high in omega-3 fatty acids) twice per week while the other half (61 women) were not. The researchers followed these women and their children from pregnancy until the children were three years old. Blood samples were obtained from the mothers during pregnancy and from the babies at birth and at age 6 and 36 months. These blood samples were used to assess EPA and DHA levels, as well as immunoglobulins and immunologic responses to determine differences in immune function and allergic responses.
A simple dietary intervention—like the addition of salmon to the weekly menu—can have profound impacts on disease progression in children.
The researchers found that dietary intervention resulted in differences in the immune systems of the two groups of children. In particular, some factors related to the development of allergies in children were lower in the babies whose mothers had consumed a steady amount of omega-3 fatty acids, in the form of salmon meals twice weekly. Still, the researchers observed no significant difference in cases of allergies and asthma between the two groups of babies at age 6 months. By 36 months, however, there was a difference between the two groups of children. The researchers found that a higher number of children whose mothers had eaten a regular, unchanged diet had developed asthma, compared to fewer children whose mothers had eaten salmon twice per week.
“These findings suggest that a simple dietary intervention—like the addition of salmon to the weekly menu—can have profound impacts on disease progression in children,” explains Dr. Calder. He plans to continue to follow the young children in this study as they grow to get a fuller picture of allergy and asthma progression over time.
Dr. Calder conducts experiments with similar dietary interventions for a variety of inflammation-related conditions including
rheumatoid arthritis
and
inflammatory bowel disease.
He strongly believes that diet is an important component in the progression of disease and urges students to make healthy, balanced meal choice to keep themselves strong. As Dr. Calder concludes: “You are what you eat.”
Dr. Philip Calder is Professor of Nutritional Immunology at the University of Southampton in England. His research focuses on the relationship between diet and disease through a variety of diet-based interventions. Dr. Calder hopes his work contributes to the improvement of diets and human health around the world. When not in the laboratory, Dr. Calder enjoys traveling, photography, listening to music, and spending time with his family.
For More Information:
- Noakes, P. et al. 2012. “Increased intake of oily fish in pregnancy: effects on neonatal immune responses and on clinical outcome in infants at 6 months.” American Journal of Clinical Nutrition, 95: 395-404.
- Miles, E. et al. 2011. “The salmon in pregnancy study: study design, subject characteristics, maternal fish and marine n-3 fatty acid intake, and marine n-3 fatty acid status in maternal and umbilical cord blood.” American Journal of Clinical Nutrition, 94(suppl): 1986S-92S.
- Calder PC. “Omega-3 polyunsaturated fatty acids and inflammatory processes: nutrition
To Learn More:
- Dr. Philip Calder website: http://www.southampton.ac.uk/medicine/about/staff/pcc.page#publications
Food Allergies
- Food Allergy Research and Education. https://www.foodallergy.org/
- American College of Allergy, Asthma, and Immunology. http://acaai.org/allergies/types/food-allergies
- Mayo Clinic. http://www.mayoclinic.org/diseases-conditions/food-allergy/basics/definition/con-20019293
Asthma
- Centers for Disease Control and Prevention. http://www.cdc.gov/asthma/faqs.htm
- American Lung Association. http://www.lung.org/lung-health-and-diseases/lung-disease-lookup/asthma/
- National Heart, Lung, and Blood Institute. http://www.nhlbi.nih.gov/health/health-topics/topics/asthma
Want to learn a lot more about the different kinds of fats? Check out this YouTube video by Dr. Calder- https://www.youtube.com/watch?v=R0AB5Alx0pE and this What A Year! story (Peanut Power) http://www.whatayear.org/10_15.php from October of 2015.
And here’s a What A Year! story on asthma (The Work of Natural Killers) from October 2006 - http://www.whatayear.org/10_06.html
Written by Rebecca Kranz with Andrea Gwosdow, PhD at www.gwosdow.com

