| |
"This really changes the way we think about asthma."
Asthma
affects nearly 20 million people in the United States alone (www.aafa.org). Obviously, anything that interferes with breathing is dangerous, and the percentage of people with asthma in the US is rising. So a discovery that gives us a better understanding of how asthma works is important to millions of patients.
An asthma attack is a response of the body's
immune system. The immune system defends the body against foreign invaders such as bacteria, viruses, and abnormal or foreign cells. This is accomplished by recognizing, attacking, destroying and eliminating the invader from the body.
If you have asthma, or know someone who does, then you are familiar with the symptoms: difficulty breathing, wheezing, a feeling that your chest is being squeezed, and spasms of coughing or gasping. Often, asthma attacks are triggered by an allergy (pollen,
dust mites, or
pet dander , for example); but an amazing number of other things can also cause them: stress, exercise, cold air, hyperventilation, smoke, or viruses. Treatments usually include prescribed steroids such as cortisone, but because asthma can be triggered by so many different agents, some people do not respond to treatment.
Dr. Umetsu focused his team's research on
the natural-killer
T (NKT) a specific cell from the immune system. To study
this cell, Dr. Umetsu and his colleagues used specially bred mice
called knockout
mice that don't have NKT-cells. These researchers tried to induce
asthma in NKT-deficient mice with different antigens
and allergens.
To their surprise, Dr. Umetsu's team
found that mice lacking NKT-cells did not develop asthma. "Our
findings were unexpected", says Dr. Umetsu, who concluded that
NKT-cells were important in the development of asthma in mice.
Next, to determine if NKT-cells were also important for the development of asthma in people, Dr. Umetsu and his colleagues took cells from the lungs of 14 patients with severe asthma and compared them to cells from the lungs of 6 people without asthma (the
control group) and to 5 people with a different lung disease called
sarcoidosis.
Cells were removed from the lungs by a
procedure
in which fluid is put into the lungs and then removed for examination. The number of NKT-cells in the sample was counted.
Interesting Result: Compared to the healthy people and the people with sarcoidosis, patients with asthma had large numbers of NKT-cells in their lungs. In other words, only patients with asthma had numerous NKT-cells in their lungs. Through these experiments, these researchers discovered that NKT-cells are specific for asthma.
So Dr. Umetsu and his colleagues concluded that NKT-cells are important in the development of asthma in some people.
"This really changes the way we think about asthma," says Dr. Umetsu, "because NKT-cells are different from other T-cells involved in asthma." Natural killer T-cells are activated by a particular type of fat called
glycolipid. Doctors had thought that an asthmatic reaction began when T-cells were activated by
proteins. In some people, at least, the asthmatic reaction may be caused by a different type of allergen than originally thought.
Part of Dr. Umetsu's ongoing research is to identify molecules in the body that may actually trigger the NKT-cells to begin an asthma attack. As it turns out, some
microorganisms
and certain plants have glycolipids that seem to activate NKT-cells. People with this type of asthma may not respond to steroids because NKT-cells do not respond to steroids.
Instead, other drugs must be developed that target NKT-cells. In order to develop these drugs, Dr. Umetsu and colleagues must learn more about the biology of NKT-cells. This research is happening right now.
The Children's Hospital researchers hope future studies will lead to the development of new drugs for the treatment of NKT-induced asthma.
| Dr. Dale Umetsu is
an immunologist
and pediatrician
whose research focuses on immune cells (T-cells and NKT-cells)
and the development of diseases like asthma and allergies.
He became interested in asthma as a medical resident, where
he saw many patients with asthma and realized this disease
was not well understood. In Boston, Dr. Umetsu is a Professor
of Pediatrics at Children's Hospital, Boston, MA. He encourages
his research team and collaborators to use their imagination
to answer questions not solved before. |
 |

Dr. Dale Umetsu |
To Learn More:
- Akbari O, Stock P, Meyer E, Kronenberg M, Siudobre S, Nakayama T, Taniguchi M, Grusby MJ, DeKruyff RH, Umetsu DT. Critical role of NKT cells producing IL-4 and IL-13 in the development of allergen-induced airway hyperreactivity. Nature Medicine. 9:582-88.
- Meyer EH, Goya S, Akbari O, Berry GJ, Savage PB, Kronenberg M, Nakayama T, DeKruyff RH, Umetsu DT. Glycolipid activation of invariant T cell receptor+ NKT cells is sufficient to induce airway hyperreactivity independent of conventional CD4+ T cells. Proceedings of the National Academies of Science 103:2782-2787, 2006.
- Akbari, O, Faul JL, Hoyte EG, Berry GJ, Wahlstrom J, Kronenberg M, DeKruyff RH, Umetsu DH. CD4+ invariant T-cell receptor+ natural killer T cells in bronchial asthma. New England Journal of Medicine 354:1117-1129, 2006.
About Asthma:
About the Immune System:
HOME | ABOUT | ARCHIVES | TEACHERS | LINKS | CONTACT
All content on this site is © Massachusetts
Society for Medical Research or others. Please read our copyright
statement — it is important.
|
|
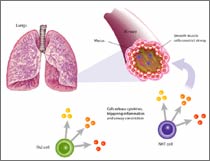
The Development of Asthma
|
A Very Concise Description of the Human Immune System
The cells of the immune system that respond
to invasion are white blood cells or leukocytes.
There are several types of leukocytes and each has a special
job to perform. During an asthma attack,
many things happen almost simultaneously in the body: macrophages
— a kind of scavenger cells — recognize the
invader (called an antigen)
and summon helper
T-cells to come fight the invader. Helper T-cells
recognize invaders by shape and chemical signals and summon
other immune cells into play, as needed.
One type of T-cell activated by helper
T-cells is called the natural killer T-cell or NKT
cell, which attacks the invading allergen
and help remove it from the body. At the same time, helper
T-cells also activate B-lymphocytes,
which make antibodies
against the allergen. Each antibody has a fingerprint that
matches a specific antigen. When an antibody encounters its
matching antigen, the antigen is "caught" and destroyed. Once
that happens, suppressor T-cells
slow down and eventually stop the immune response
|
Sign Up for our Monthly Announcement!
...or  subscribe to all of our stories! subscribe to all of our stories!

What A Year! is a project of the Massachusetts Society for Medical Research.
|
|

