| |
A fourteen-year old boy is admitted to the hospital with severe
heart failure
. A
heart transplant
could save his life. But there are several obstacles in the way of this potentially life-saving procedure. First, the demand. According to the National Institutes of Health, approximately 3,000 people are on the waiting list for a heart transplant on any given day, and
about 2,000 hearts are available for transplant in a given year. Wait times can last from days to months.
To ease this first hurdle, a
Total Artificial Heart
is available to help patients stay alive long enough to receive a transplant.
Pediatric patients face an additional obstacle, however, because children and young adults come in all different sizes. Until doctors attempt a transplant procedure of the device, there is no way to know whether it will fit. In the case of the fourteen-year old boy, doctors completed the transplant of the Total Artificial Heart, but there were complications. A new procedure, however, used medical imaging and computer models to determine what was causing the complications, and doctors were able to implant the device successfully. This procedure, called a Virtual Implant, has the potential to revolutionize implantation procedures for patients big and small.
“It was a simple idea.” We thought, “Wouldn’t it be better to use a three-dimensional model of a three-dimensional patient?”
The Virtual Implant was developed by a team of researchers at Arizona State University led by Dr. David Frakes and Justin Ryan, a doctoral student in Dr. Frakes’ laboratory. “It was a simple idea,” explained Dr. Frakes.
Previously, doctors had been using two-dimensional images to determine whether a three-dimensional object would fit into a three-dimensional space. They would draw a line between the
spine
and the
sternum
and use this measurement as the basis for the procedure. We thought, “Wouldn’t it be better to use a three-dimensional model of a three-dimensional patient?” And the idea for the Virtual Transplant was born. “We take a computer model of the medical device and place it into a computer model of the human patient and see what happens,” explained Dr. Frakes. “That’s it.”
The two main components of the procedure are a model of the human patient and a model of the medical device. The model of the human patient is produced using medical images obtained from technologies such as
Magnetic Resonance Imaging (MRI)
or
Computed Tomography (CT)
. These images take pictures in layered slices of three-dimensional space that provide the basis for a three-dimensional computer model. The model of the medical device can be obtained using simpler technology because only the physical shape of the device is necessary to determine whether it will fit inside the patient. Dr. Frakes and his team used laser scanners to create the computer model of the device.
Once the two computer models have been created, Dr. Frakes and his team enlist the help of the doctors in charge of the procedure to implant one computer model (the device) into another (the patient). This is a Virtual Implant because no actual device or actual patient is involved. With better models, the doctors can more accurately determine whether a device will fit into a given patient, and also the best way to implant the device. Since the doctors performing the virtual implant are the same ones who will conduct the actual procedure, the Virtual Implant acts as a trial run and can greatly improve surgical outcomes. After the procedure, the researchers follow up with the doctors to see how closely the surgeons were able to implant the device as planned, and also follow patients in the event of complications.
Currently, the Virtual Implant has been successfully used in ten cases of pediatric patients with
congenital heart defects. The possibilities, though, are limited only by the imagination. “In pediatric patients, the most pressing question is whether the device will fit,” explained Dr. Frakes. “But there are plenty of applications for adult patients too.” In adults, doctors know the device will fit, but there is still a question of the best way to implant the device. Sometimes doctors will disagree on how to best complete a procedure. A virtual implantation can help doctors figure out in real space how to proceed. With the success of the Virtual Implant in children with heart problems, Dr. Frakes and his team are planning to expand the procedure for use in adult cardiac patients as well.
In addition to the Virtual Implants, Dr. Frakes and his team are also using a new technology called a 3D printer to turn their computer models into physical objects.
In addition to the Virtual Implants, Dr. Frakes and his team are also using a new technology called a 3D printer to turn their computer models into physical objects. Rather than ink, the printer users materials like plastic or metal to construct a three-dimensional object one layer at a time. In this way, Dr. Frakes and his team can use medical images to create 3D models of a patient’s heart, and eventually other body parts as well. These model hearts are additional tools doctors can use to improve patient outcomes.
Dr. David Frakes is an Associate Professor in the Schools of Biological and Health Systems Engineering and Electrical, Computer, and Energy Engineering at Arizona State University. He is an electrical engineer by training, and decided to use his skills in image processing to help people stay healthy. His advice to students is to find a problem you really want to change, and then find a solution. That process of exploration can encompass many fields and specialties. “Our work is by definition interdisciplinary,” remarked Dr. Frakes. Dr. Frakes is also an accomplished pole-vaulter. He has an Olympic-standard pole-vaulting facility in his backyard, and you can find him there when he’s not in the laboratory.
Justin Ryan is a doctoral student in biomedical engineering in the School of Biological and Health Systems Engineering at Arizona State University. Ryan conducts his research in the laboratory of Dr. David Frakes.
To Learn More:
- Park, S. et al. 2014. “Total artificial heat in the pediatric patient with biventricular heart failure.” Perfusion, 29(1): 82-8
- Kantrowitz, A. 1998. “America’s First Human Heart Transplantation.” American Society for Artificial Internal Organs Journal.
For More Information:
- American Heart Association. www.heart.org
- Texas Heart Institute. texasheart.org/HIC/Topics/Proced/hearttx.cfm
- Nova Online: Operation Heart Transplant. www.pbs.org/wgbh/nova/eheart/transplant.html
- Heart in Your Hand. heartinyourhand.biz
- Heartprint. biomedical.materialise.com/heartprint
Written by Rebecca Kranz with Andrea Gwosdow, PhD at www.gwosdow.com
HOME | ABOUT | ARCHIVES | TEACHERS | LINKS | CONTACT
All content on this site is © Massachusetts
Society for Medical Research or others. Please read our copyright
statement — it is important. |
|
|


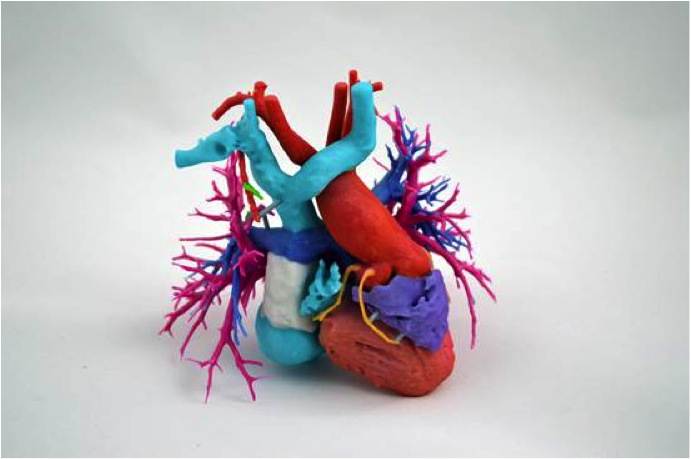
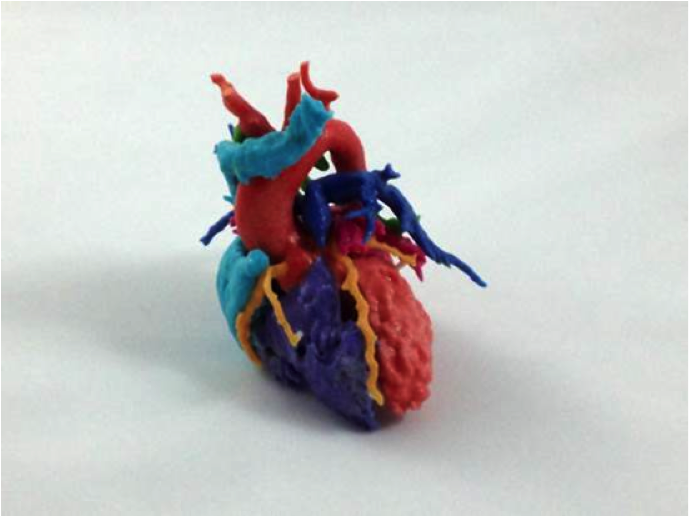
3D printed heart

A computer-generated image of a patient with an implanted artificial heart

Dr. David H. Frakes

Researcher Justin Ryan removes excess material on the heart model with a brush.

A 3D printer in action … creating a Yoda statute
http://www.youtube.com/watch?v=8_vloWVgf0o
Sign Up for our Monthly Announcement!
...or  subscribe to all of our stories! subscribe to all of our stories!

What A Year! is a project of the Massachusetts
Society for Medical Research.
|
|

