| |
How many of you have ever been hit in the head? An incoming soccer or basketball you thought you could get, a mistaken wander through a game of catch on the playground, a car or bicycle accident, or falling off the swing set or monkey bars- the list goes on and on. Most of us recover quickly from such frequent accidents, but a blow to the head is no laughing matter. New research by Dr. Charles Wilkinson and colleagues from the Veterans Affairs (VA) Puget Sound Health Care System and University of Washington shows that even incidents that seem minor could have important, long-lasting effects on your health.
Here are some brain-bouncing statistics on head injuries: According to the Centers for Disease Control and Prevention, an estimated 1.7 million people sustain a traumatic brain injury every year resulting in approximately 52,000 deaths and 275,000 hospitalizations. Emergency rooms across the country treat over 600,000 patients of all ages for traumatic brain injury, nearly three-quarters of them aged 0-14 years. In fact, traumatic brain injuries are a contributing factor to nearly a third of all injury-related deaths in the United States, and two of the most susceptible groups are children 0-4 years and adolescents 15-19 years.
Traumatic Brain Injury
So, what is traumatic brain injury? Traumatic brain injury, or TBI for short, refers to any brain injury caused by external force that results in some loss of function, no matter how temporary.
The most familiar and frequent traumatic brain injury is a
concussion,
which generally occurs as a result of a blow or jolt to the head or body that causes the brain to rapidly move back and forth against the skull. Concussions comprise approximately three-quarters (75%) of all such injuries. They are considered to be a mild TBI, as are other TBIs that do not penetrate the skull or cause loss of consciousness for more than 30 minutes.
Common causes of concussions include falls, collisions and traffic accidents. In children and adolescents in particular, concussions are often related to sporting and recreational activities. Movement of the brain in the skull as a result of a TBI can damage brain cells and other brain tissue and create chemical imbalances in the brain. Often TBIs can seem so minor: the pressure to stay in the game or on the trail is so great, that we do not take the time to let our bodies and minds recover from the injury. Although the majority of TBIs will heal with time, new research by Dr. Wilkinson suggests that the consequences of TBIs may be much longer-lasting than we previously thought.
Hormones Connected to TBI
Dr. Wilkinson has spent his career studying the effects of
hormones,
particularly stress hormones, on
neurological diseases
such as
Alzheimer's disease,
Parkinson's disease,
depression,
and normal aging.
Hormones are chemicals that travel through the blood stream from the part of the body where they are secreted and flow to the part of the body they are intended to affect.
Hormones and the glands that produce them are collectively known as the
endocrine system.
Some hormones you may have heard of include
insulin
one of several hormones implicated in the development of
diabetes
and sex hormones like
estrogen
and
testosterone.
You are probably equally familiar with stress hormones, which regulate your response to internal and external stressors, although you may not know them by name. Dr. Wilkinson has found important relationships between the hormones involved in our stress response and the development of many neurological diseases.
Hormones are not the first things that come to mind in the case of traumatic brain injury. This was one of Dr. Wilkinson's first thoughts when a colleague, Dr. Elaine Peskind, suggested that he try to design a project examining the relationship between hormones and TBI. As he began his background research, however, Dr. Wilkinson found several studies that suggested a high prevalence of hormone abnormalities in patients who had sustained a TBI. In particular, previous experiments suggested that hormones secreted by the
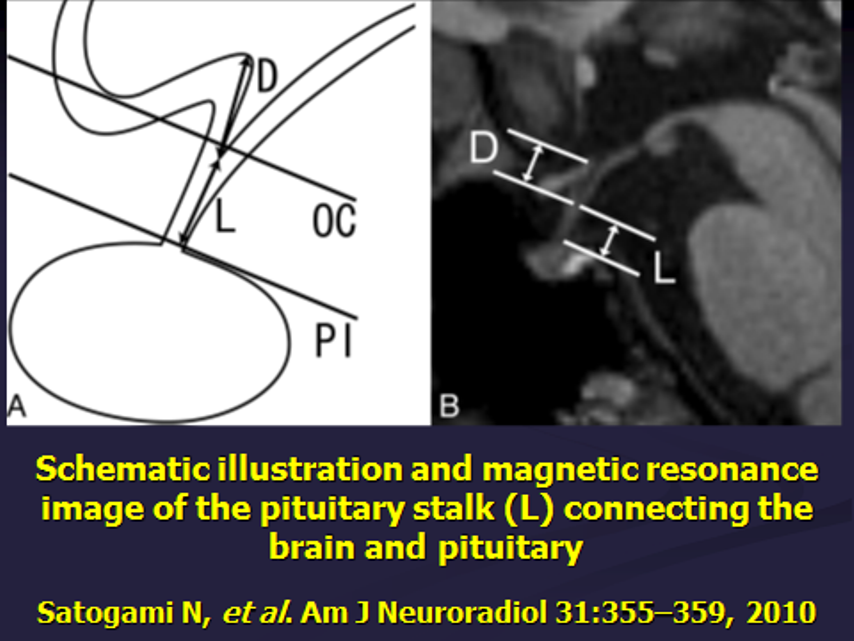
pituitary gland
in the brain might be most affected. The pituitary gland is a small, garbanzo bean-like structure located very deep inside the brain, which is attached to the cerebral structures above by a tiny stalk. The location of the pituitary gland makes it particularly vulnerable to any type of shaking as a result of a TBI. Given that hormones produced by the pituitary gland are vital to growth, metabolism, and sexual function, Dr. Wilkinson now suggests that abnormal hormonal levels as a result of TBI may be a missing link in our understanding of their long-term consequences.
Pituitary Gland
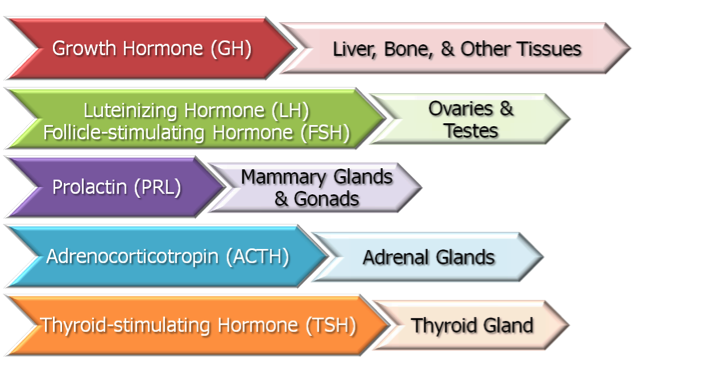
Pituitary Gland Hormones And The Organs They Target
Military Veterans with TBIs
For their research, Dr. Wilkinson and his colleagues worked with veterans who had experienced a type of TBI called a blast concussion. Blast concussions are referred to as mild TBI because there is no penetration of the skull, but they can still have very serious consequences. Rather than a single, local impact to the head generally associated with TBIs, blast forces hit the entire body including the head, causing a rapid acceleration and deceleration of the brain. In a military situation, the blast could occur multiple times as it bounces off of vehicles or other surrounding structures and hits the person again. 'Blast concussions are a deceptive injury,' explains Dr. Wilkinson, 'because they can cause a lot of damage without the person realizing what has happened.'

IED Explosion
In order to understand the long-term effects of blast concussions, Dr. Wilkinson and his team advertised for volunteers who had served in Afghanistan or Iraq, where blast concussions have become the 'signature injury' of combat. The researchers compared two groups of veterans: those who had experienced at least one blast concussion and a control group who had experienced the same type of traumatic situation but had not sustained a blast concussion. In this way the researchers hoped to identify differences between the two groups that could be attributed to the blast concussion itself as opposed to the situation in which the concussion occurred. Dr. Wilkinson and his team took blood samples from both groups and compared their levels of a variety of hormones. They found that veterans who had sustained a blast concussion during combat were more likely to exhibit hormone abnormalities that have some of the same symptoms as
post-traumatic stress disorder,
depression, and other physical and mental illnesses.
TBIs and Growth Hormone
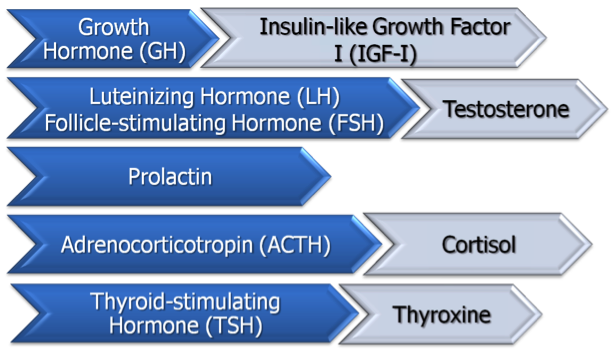
Pituitary Gland Hormones
In particular, the researchers noted increased abnormalities in
growth hormone,
the hormone responsible for stimulating physical growth in children and adolescents. It seems counterintuitive at first that growth hormone would be most affected by TBIs: these are adults who are no longer growing so what difference would it make whether their growth hormone levels were decreased? It turns out that growth hormone deficiency in adults has important consequences for learning, memory, and mood changes. These are symptoms that would not necessarily be attributed to growth hormone. In addition, these hormonal abnormalities result in changes in body composition: muscle loss, bone loss, fat deposition, and other changes that can lead to increased cardiovascular problems.
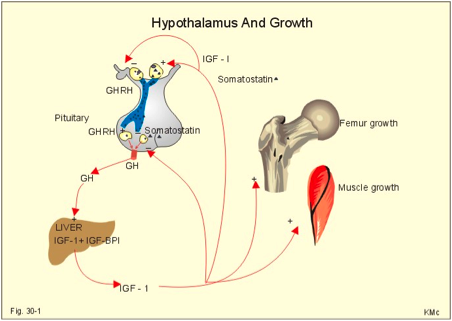
Insulin-like Growth Factor (IGF-1) and Growth Hormone
Dr. Wilkinson refers to growth hormone deficiency as the
Catch 22
of all pituitary gland disorders. On one hand, it is the most common because the cells that produce growth hormone are in the outer, most exposed region of the pituitary gland. On the other hand, growth hormone deficiency is least likely to be treated because many of the problems it can cause such as learning and memory, mood changes, cardiovascular problems, and more are not generally considered hormone-related and, in most cases doctors are not looking for hormonal abnormalities after a brain injury.
One of the most important contributions of Dr. Wilkinson's research, then, is to educate doctors, particularly those treating veterans, to consider hormone abnormalities when treating patients who have sustained TBIs.
While some hormone abnormalities can be identified by measuring blood levels of hormones, growth hormone deficiency requires stimulation of growth hormone cells to see if they respond properly.
It is important to note that Dr. Wilkinson is not a physician and cannot diagnose veterans. He does, however, refer veterans with abnormal hormonal profiles to appropriate doctors for further medical attention. Dr. Wilkinson strongly believes that greater awareness of the connection between hormone abnormalities and TBIs could go a long way toward appropriate diagnosis and treatment of a variety of problems that do not seem to be related.
What Next?
There are many avenues that Dr. Wilkinson hopes to explore in future research. Most immediately, Dr. Wilkinson and his colleagues would like to correlate particular brain injuries with specific hormone profiles. Results from this type of inquiry could enable doctors and researchers to better understand the differential effects of TBI depending on the type and cause of injury. In addition, all of the experiments on blast concussions conducted so far have only included men. This is in part because the majority of veterans, including those who have sustained blast concussions, are men. As more women are deployed into combat situations, however, Dr. Wilkinson also hopes to conduct similar studies with women.
Finally, what does this research on blast concussions in veterans have to do with that minor TBI you sustained on the soccer field? It means that we--all of us including parents and children, coaches and athletes, and everyone in between need to be more vigilant about preventing, recognizing, and treating concussions and other traumatic brain injuries. Just because a TBI seems to resolve itself does not mean that all is necessarily well. Protecting your brain can go a long way towards maintaining good mental and physical health.
Dr. Charles Wilkinson is Research Physiologist in the Geriatric Research, Education and Clinical Center of the VA Puget Sound Health Care System and Research Associate Professor in the Department of Psychiatry and Behavioral Sciences at the University of Washington School of Medicine. His research is funded by the Departments of Defense and Veterans Affairs.
Dr. Wilkinson first became interested in psychology and studying the mind after reading the psychological thriller Crime and Punishment during college. As he took more psychology courses, he became more interested in what was actually going on at a biochemical level, how brain function related to behavior. He has spent his career examining the effects of stress hormones on the development of neurological disorders. His most recent research focuses on hormone abnormalities as a result of traumatic brain injury. When not in the laboratory, Dr. Wilkinson enjoys reading, going to the theater, traveling, and spending time with family.
For More Information:
- Wilkinson, C. et al. 2012. 'High prevalence of chronic pituitary gland and target-organ hormone abnormalities after blast-related mild traumatic brain injury.' Frontiers in Neurology, 3: 1-12. Accessible from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3273706/pdf/fneur-03-00011.pdf
- 'Traumatic Brain Injury in the United States.' 2010. Centers for Disease Control and Prevention.http://www.cdc.gov/traumaticbraininjury/pdf/blue_book.pdf
To Learn More:
Traumatic Brain Injury
- Centers for Disease Control and Prevention. http://www.cdc.gov/TraumaticBrainInjury/index.html
- National Institute of Neurological Disorders and Stroke. http://www.ninds.nih.gov/disorders/tbi/tbi.htm
Childhood TBIs and Concussions
- National Dissemination Center for Children with Disabilities. http://nichcy.org/disability/specific/tbi
- 'Concussion in Sports.' Centers for Disease Control and Prevention. http://www.cdc.gov/concussion/sports/recognize.html
- 'Heads Up: Concussion in Youth Sports.' Centers for Disease Control and Prevention. http://www.cdc.gov/concussion/HeadsUp/youth.html
TBIs and the Military
- 'TBI & the Military.' Defense and Veterans Brain Injury Center. http://www.dvbic.org/about/tbi-military
- 'Blast Concussions.' Defense and Veterans Brain Injury Center. http://www.dvbic.org/blast-injuries
- Brain Trauma Foundation. https://www.braintrauma.org/tbi-faqs/military-tbi/
- 'Traumatic Brain Injury: What Military Families Need to Know.' Center for the Study of Traumatic Stress. http://www.cstsonline.org/wp-content/resources/CTC_TBI_patient.pdf
- 'DoD Worldwide Numbers for TBI.' Defense and veterans Brain Injury Center. http://www.dvbic.org/dod-worldwide-numbers-tbi
TBIs and the Endocrine System
- "Traumatic Brain Injury.' Hormone Health Network." http://www.hormone.org/questions-and-answers/2013/traumatic-brain-injury
- 'Head Injury and Hypopituitarism.' http://www.headinjuryhypo.org.uk/
Written by Rebecca Kranz with Andrea Gwosdow, PhD at www.gwosdow.com
HOME | ABOUT | ARCHIVES | TEACHERS | LINKS | CONTACT
All content on this site is © Massachusetts
Society for Medical Research or others. Please read our copyright
statement — it is important. |
|
|
 Wilkinson Lab Team
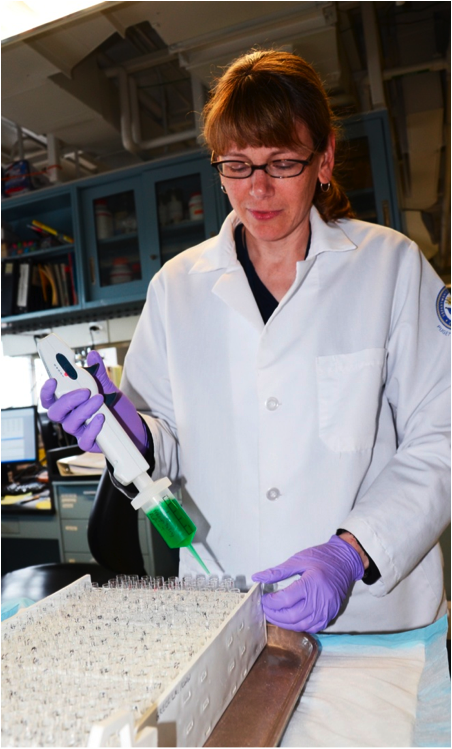 Elizabeth "Libby" Colasurdo
 Carl Sikkema
Head Trauma Interview with Dr. Wilkinson
Great Science Sites
NIH | High School
NIH | Middle School
ACS | Science for Kids
SciAm | Blog
Sign Up for our Monthly Announcement!
...or  subscribe to all of our stories! subscribe to all of our stories!

What A Year! is a project of the Massachusetts
Society for Medical Research.
|
|

