| |
As the Queen stitched, snowflakes
falling outside the window distracted her, and the needle suddenly
pricked her finger. Three drops of bright red blood fell on the
white snow outside! The Queen said to herself, ‘How nice
it would be to have a pretty child, white as snow and rosy as
the red blood.” Lo and behold, Snow White then was born.
Of course, the Queen never thought about how that pinprick in
her skin would be put together again. She just kept on stitching.
All she knew was that within a few hours the pinprick would be
gone. While she was embroidering, though, her body was working
to make sure the tiny hole in the Queen’s hand was rapidly
repaired.
Actually, many steps are involved in plugging-up
even the tiniest of pinpricks in a finger. The initial plug,
or blood clot, is initiated by platelets that circulate in the
blood specifically for that purpose. Then there are many different
proteins, called clotting factors, which contribute to stop the
bleeding through the complex process of coagulation. These proteins
include Factors I through XIII, protein C, protein S, von Willebrand
Factor, and antithrombus III. They must work in a highly cooperative
manner to do the job. To give you an idea of just how well-coordinated
this process of coagulation is, look at the diagram below from
the article on coagulation in Wikipedia:
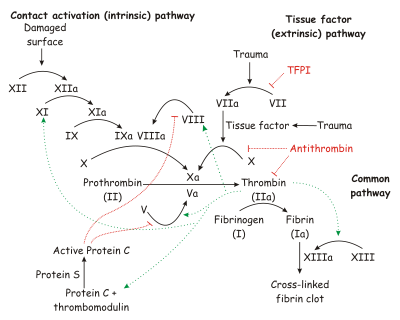
http://en.wikipedia.org/wiki/Coagulation#The_coagulation_cascade
While we all take blood clotting for granted,
if any one of the critical coagulation factors is missing,
the consequences can be deadly. For instance, deficiency of
Factor VIII or IX leads to conditions known as Hemohilia A
and B, respectively.
Boys
vs. Girls
Overall, hemophilia is rare (about 20,000 people in the
US have the condition) but Hemophilia A is by far the most common
type of the disease. It is estimated that one out of every five-
to ten-thousand males in the US cannot make sufficient quantities
of Factor VIII, which is crucial to the creation of a successful
clot. Without Factor VIII, the body is unable to plug the hole
fully, and as a result the person may keep bleeding indefinitely.
There are different levels of severity depending on how much, or
how little, Factor VIII the body is able to produce. In the most
severe cases, even a pinprick could possibly prove deadly.
There are many reasons why sufficient amounts of Factor VIII
may not be produced. The gene that makes Factor VIII is located
on the X chromosome. Therefore, mutations in the gene encoding
Factor VIII are inherited through the X chromosome and can
be passed only from mother-to-child. If the child is female,
she has two X chromosomes, so it does not matter if only
one of the X chromosomes carries the Factor VIII mutation.
In this situation, she will not suffer from hemophilia. She
is known as a carrier of hemophilia because the affected
chromosome can be passed on to her child. But if the child
is male, he will inherit the X chromosome from his mother
and the Y chromosome from the father, so the only copy of
Factor VIII gene he receives will be the defective one from
the hemophilia carrier mother. That is why only males suffer
from the consequences of Hemophilia A.
People with Hemophilia A are unable to properly make blood
clots due to the lack of Factor VIII. Even minor injuries may
result in excessive bleeding and, without prompt medical attention
and administration of Factor VIII, the person may die from
blood loss. It is for this reason that hemophilia can be a
dangerous disease if a person is unaware of it, and hemophiliacs
need to carefully avoid trauma. While there are treatments
to induce clotting in hemophiliacs, there is no known cure
for Hemophilia A.
Of course, people with hemophilia can and do encounter injuries
just like non-hemophiliacs: they break bones and require various
types of surgery. A lot of work has been done over decades
to understand the role of Factor VIII, including determining
where in the body Factor VIII is made. Interestingly, it had
been noted that hemophiliacs who received liver transplants
were suddenly cured of their hemophilia.
The liver has several types of cells and
it was unclear which one of these cells was most important for
producing and releasing Factor VIII. This is where Dr. Sanjeev
Gupta of the Albert
Einstein College of Medicine in New York comes in. “These
cases and evidence from previous studies suggested that something
important was happening with Factor VIII and liver cells,” said
Dr. Gupta, a Professor of Medicine and Pathology, and an expert
in hepatology. “We
decided to investigate.”
The Liver: There's More to It Than You Think
The liver is
the largest internal organ in the human body and serves many important
functions. It is responsible for metabolism, or processing of food
you eat into energy you can use. The liver synthesizes many proteins,
including those that circulate in the blood. It makes bile, which
is secreted into the small intestine to help with digestion. The
liver processes various chemicals, drugs and toxins to make them
safe for the body. So overall, the liver is responsible for regulating
blood sugar, amino
acid and lipid levels,
and synthesizing cholesterol,
sugars and proteins, as well as removing drugs or toxins.
The liver is made up of many cell types. Two main types of liver
cells are epithelial
cells, or hepatocytes, and sinusoidal
endothelial cells. Endothelial cells form the lining of the
blood-filled spaces of the liver and possess highly specialized
functions, including production of growth factors or cell signaling
molecules, as well as scavenger functions required for incorporating
specific substances.
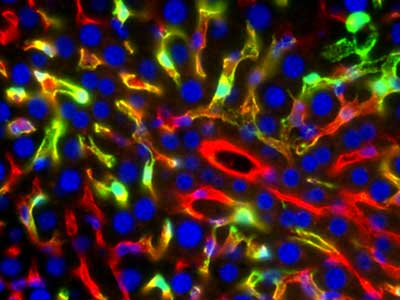
This
figure demonstrates transplanted liver sinusoidal endothelial
cells (LSEC) after these cells integrated and proliferated in
sinusoidal spaces of the mouse liver. Transplanted LSEC are in
green color, which was produced by immunostaining for Green Fluorescent
Protein (GFP) in transplanted LSEC. GFP protein will have been
produced in only endothelial cells because its expression was
regulated by the Tie-2 promoter, which is active in only endothelial
cells. Native LSEC are in red color due to immunostaining for
the CD31 marker of endothelial cells. On occasion, transplanted
LSEC appear to be yellow due to overlapping green and red colors
from GFP and CD31 expression in cells.
Dr. Gupta initially
hypothesized that hepatocytes were making Factor VIII because
of their wide variety of roles in the liver. To test this hypothesis,
Dr. Gupta used a mouse model of Hemophilia A where the Factor
VIII gene had been disrupted by DNA recombination methods or “knocked
out ” from the genome.
Liver cells in these animals were healthy except that they did
not make Factor VIII. Dr. Gupta’s team then injected
these hemophilia mice with normal hepatocytes to see if they
would begin to produce Factor VIII. They did not.
So That Didn't Work. What Do We Do Now?
So, contrary to what Dr. Gupta had initially expected, transplantation
of healthy hepatocytes did not have an effect on Factor VIII
levels in hemophilia mice. “I
was surprised,” said Dr. Gupta. “But I knew that
hepatocytes were not the only option. It was possible that endothelial
cells were making Factor VIII, or that Factor VIII was being
produced by something different.” Dr.
Gupta and his team then examined the capacity of cells other
than hepatocytes (specifically, liver sinusoidal endothelial
cells) and found that Factor VIII appeared in the blood of mice
after transplantation of these cells. This was the first clue
that transplantation of liver sinusoidal endothelial cells might
be capable of correcting Hemophilia A.
In
the next step, Dr. Gupta and his team determined whether liver
endothelial cells could be replaced by transplanted cells. The
effort was to develop suitable ways to have transplanted cells
survive and proliferate in
the liver, which was their natural home. This required a
series of studies in mice with genetically marked cells from
donor mouse livers. The goals of these studies were to identify
transplanted cells and to create sufficient room in the recipient
liver for transplanted cells to proliferate. Dr. Antonia
Follenzi and other members of the team were successful in
establishing that transplanted liver endothelial cells survived,
proliferated, and functioned normally after the liver had
been injured by a particular chemical. They then studied
Factor VIII production from liver sinusoidal endothelial
cells by injecting hemophiliac mice with endothelial cells
from normal, healthy mice. “This time,” said
Dr. Gupta, “large amounts of Factor VIII appeared in the
blood stream and were maintained at high levels indefinitely.” Moreover,
hemophiliac mice acquired the capability to stop bleeding.
In other words, transplanted liver endothelial cells were
producing Factor VIII and mice treated with healthy cells
had been cured of hemophilia.
“This
is a huge finding,” remarked Dr. Gupta. We can now
add Hemophilia A to the list of diseases that can be cured
by liver cell therapy. This means that one day we will be
able to inject people with Hemophilia A with healthy endothelial
cells and restore the capacity of their livers to produce
Factor VIII. This could be a lifesaver for many hemophiliacs.
Perhaps one day hemophiliacs will be able, like the Queen,
to go on stitching while that pinprick disappears.
This principle
of replacing liver endothelial cells needs additional work before it can be
used in clinical human medicine, although it represents a major advance in
the area of tissue and organ transplantation
Dr. Gupta is Professor of Medicine and Pathology and
Dr. Follenzi is Instructor of Pathology at Albert Einstein College
of Medicine in New York. Their major area of research is liver-directed
cell and gene therapy.
|
|
|
 Dr. Sanjeev Gupta Dr. Sanjeev Gupta
 Dr.
Antonia Follenzi Dr.
Antonia Follenzi
 How
Clotting Works How
Clotting Works
Sign Up for our Monthly Announcement!
...or  subscribe to all of our stories! subscribe to all of our stories!

What A Year! is a project of the Massachusetts
Society for Medical Research.
 You Can Be A Star - Living with hemophilia You Can Be A Star - Living with hemophilia

|
|

