| |
Let’s
take a trip back in time for a moment to the 1860’s, when
the United States was in the midst of a war. With nearly 620,000
casualties, the Civil War took a greater toll of American life
than any other war. Of those casualties, though, only one-third
died of battle wounds. The rest died of infection
and disease.
Most of the fatal illnesses resulted from the lack of sanitation
in the Civil War era. The soldiers could fight each other, but
they stood no chance against bacteria:
the invisible army.
Most bacteria are harmless because your
body can fight them off using the power of your immune
system . Some are even beneficial, like the E.
coli that naturally live in your gut to aid in digestion.
Many, however, can be deadly. Good or bad, harmful or not,
bacteria are everywhere. They are on the food you eat and
in the water you drink. They are even on your skin, just waiting
for the chance to infect you. Luckily, your skin is a barrier
that does a pretty good job of keeping them out. However,
when you scrape your knee or cut your finger, or in the case
of the Civil War, get a bullet in your leg, it breaks the
barrier and provides the perfect opportunity for the bacteria
to jump on in.
For this reason, your body has fast-acting systems to prevent
a bacterial invasion and plug the hole. You are probably very
familiar with these systems from your own experience. Here is
insight into how they work: for a smaller wound, after a few minutes
your cut stops bleeding and the next day there is a scab
over it . As your blood clotted to stop the bleeding, your
immune system also responded to prevent infection. This month
we are going to focus on the immune response.
Why do you bleed after you’ve cut your finger or scraped
your knee? Bleeding is a sign of a broken blood vessel. Blood
vessels transport blood from your heart to every part of your
body and back again. If bacteria get into your blood stream, infection
can spread to your entire body. This is called sepsis and, if
untreated, can be fatal.
Blood contains different types of blood cells: red
blood cells and white blood cells. White blood cells are also
called leukocytes. In the event of a broken blood vessel, the
white blood cells (leukocytes) are the first to “notice”
the injury before the red blood cells work to repair it. How do
the white blood cells know where to go?
Blood vessels all have a thin inner layer of special cells called
endothelial
cells. The layer itself is called the endothelium.
When you cut or scrape yourself and a blood vessel is broken,
it sets off an immediate response by the endothelial cells.
Endothelial cells store little granules of a protein called P-selectin.
When a blood vessel is broken and the endothelium is disturbed,
these ready-made granules of P-selectin are released. P-selectin
is sticky, so it slows down the white blood cells that are
flowing through the blood vessel enough for them to notice
special chemicals called chemoattractants. They guide leukocytes
to the site of the injury. Another chemical, called integrin,
stops the white blood cells so they can flatten and crawl through
the vessel wall where they will engulf any bacteria and eliminate
them from the body to prevent infection. At the same time,
chemicals responsible for blood clotting plug up the hole.
Once the hole is filled, bacteria can no longer get in. So
this is the two-part system: trap invading bacteria and close
the wound.
Dr. Denisa Wagner of the Immune Disease Institute and Harvard
Medical School studies the role of P-selectin in the immune response.
In her research, Dr. Wagner has found that
P-selectin is stored in granules called Weibel-Palade
bodies that reside in endothelial cells. To test the
importance of P-selectin in the immune response, Dr. Wagner and
her team of researchers created mice that lack the P-selectin
molecule in their endothelium. These mice are called knock-out
mice because the gene that encodes for the protein P-selectin
has been knocked out. Dr. Wagner and her team of researchers used
a technique called intravital microscopy to watch blood
flowing through the mice’s blood vessels while they slept
under anesthesia. They found that white blood cells do not slow
down at an injured site in P-selectin-deficient mice. [  A film of this intravital microscopy can be linked to on her website].
If the white cells don’t slow down, they cannot effectively
perform their anti-bacterial function.
A film of this intravital microscopy can be linked to on her website].
If the white cells don’t slow down, they cannot effectively
perform their anti-bacterial function.
So the presence of P-selectin is crucial to helping us fight
off bacterial infection. But like
most things about our bodies,
it is important to have the right amount of P-selectin. Too
little
exposes us to one kind of risk; as you’ll see below,
having too much puts us at risk in a
different way.
There are no known humans who lack P-selectin. But if there is
an excess of P-selectin, white blood cells will congregate around
the site and restrict blood flow. Humans can develop this condition.
If it occurs near the heart, it could induce a heart
attack; if it occurs near the brain it could induce a stroke.
Both are often fatal. Several drug companies are now in the process
of creating drugs that could inhibit P-selectin (called P-selectin
inhibitors) and thus reduce the risk of heart attack and stroke.
They are also working on a test for P-selectin levels in the blood
to determine a person’s risk for heart disease and stroke.
The effects of excess P-selectin can occur if the endothelium
becomes irritated by something other than a wound. There are many
ways this could happen. Two of the most common ways are through
smoking and eating a high-fat diet.
When the chemicals in cigarettes enter the blood stream, they
irritate the endothelium on the inside of the blood vessels. Upon
irritation, the endothelial cells release P-selectin, just as
they would have if the blood vessel had actually been damaged.
As a result, the white blood cells come to the injured site even
though there are no bacteria. They flatten and attach themselves
to the endothelium where they can restrict blood flow. This is
why smokers have a much higher risk of having a heart attack or
stroke.
Too much fat in the blood stream will irritate the endothelium
in the same way as smoking and cause the release of P-selectin.
Then the white blood cells come and engulf
the fat cells as they
would engulf bacteria. The white blood cells become full of fat
and look like foam. Really they are white blood cells with lots
of fat in them. Since they cannot break down the fat, they become
very large. The enlarged white blood cells activate the immune
response, indicating damage even though they are just enlarged.
The enlarged cells may release the fat into the bloodstream as
crystals. The walls of the blood vessel sense injury and try to
repair themselves by building up their walls with smooth muscle
cells. This causes the blood vessel to become narrow. Narrowed
blood vessels do not allow adequate oxygen and nutrients to the
tissues and can cause pain, which can eventually lead to a heart
attack or stroke. For this reason people who are overweight or
people who have too much fat in their diet have an increased chance
of having a heart attack or a stroke.
Smoking and eating a high-fat diet are two ways to badly manipulate
an immune system that works extremely well. The time between the
initial injury and the release of P-selectin and the flagging
of the white blood cells takes seconds. This is the body’s
preliminary measure to prevent infection. The longer a wound is
open, the more time bacteria have to get into your body and infect
you. It is equally important that you clean a wound to prevent
bacteria that are already present from getting any further into
you. Medicine has come a long way in understanding the body’s
natural disease-prevention mechanism since the Civil War.
Dr. Denisa Wagner is a Professor of Pathology
at Harvard Medical
School. She researches
P-selectin and its role in immune response
at the Immune Disease Institute and Harvard Medical School. Originally
from the Czech Republic, Dr. Wagner has been interested in biology
since her first science class in middle school. She attended college
in Geneva, Switzerland and graduate school at MIT before coming
to the Immune Disease Institute and Harvard Medical School.
|
|

The Wagner Lab Researchers
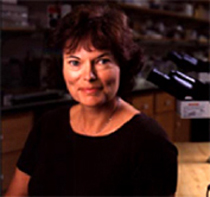
Dr.
Denisa D. Wagner
"Rolling"
Leukocytes

A
Civil War Hospital


Sign Up for our Monthly Announcement!
...or  subscribe to all of our stories! subscribe to all of our stories!

What A Year! is a project of the Massachusetts
Society for Medical Research.
|
|
| |
To Learn More:
- Dong ZM, Brown AA, Wagner DD. Prominent
role of p-selectin in the development of advanced atherosclerosis
in apoE-deficient mice. Circulation 2000;101:2290-2295.
- Dong ZM, Wagner DD. Leukocyte-endothelium
adhesion molecules in atherosclerosis. Journal of Laboratory
and Clinical Medicine 1998;132:369-375.
- Frenette, PS, Wagner, DD. Adhesion molecules--Part
II: Blood vessels and blood cells. New England Journal of
Medicine 1996;335:43-45.
- Mayadas, TN, Johnson, RC, Rayburn,
H, Hynes, RO, Wagner, DD. Leukocyte rolling and extravasation
are severely compromised in p selectin-deficient mice. Cell
1993;74:541-554.
Rebecca
Kranz with Andrea Gwosdow, Ph.D.
HOME | ABOUT | ARCHIVES | TEACHERS | LINKS | CONTACT
All content on this site is © Massachusetts
Society for Medical Research or others. Please read our copyright
statement — it is important.
|
|
|
|

