Highlights
- Fetal Atrioventricular (AV) block is one of the most life-threatening congenital heart defects and affects the rhythm of the heart, which results in a very low heart rate.
- This medical team adopted a method called the EXIT (ex-utero intrapartum treatment) to deliver a premature fetus with AV block and heart failure.
- This baby is now one year old, and with the careful attention of cardiologists, is expected to live a long, happy life.
Did you know that even unborn babies can develop heart problems? Heart problems that develop while the fetus is still in the mother's womb are known as
congenital heart defects.
The Centers for Disease Control and Prevention estimate that congenital heart defects affect
approximately 40,000 babies per year
in the United States.
Fetal Atrioventricular (AV) block
is one of the most life-threatening congenital heart defects. The problem is not with the structure of the heart, but rather, the rhythm of the heart that results in a very low heart rate. The normal fetal heart rate is 120-160 beats per minute (bpm), and with AV block the heart rate is usually less than 60-70 bpm.
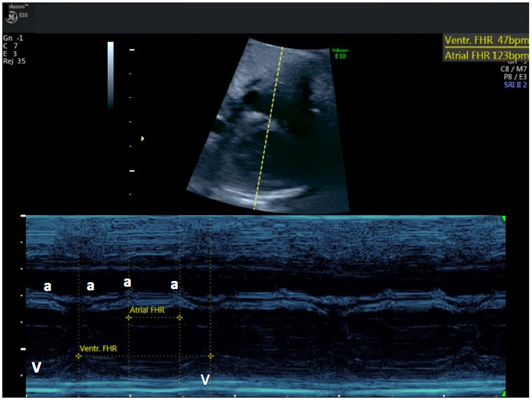
Figure 1. This is a M-Mode echocardiogram that shows the contractions of the atrium on the top (a-waves) and the contractions of the ventricle on the bottom (v-waves). Normally the atrial ventricular contractions should be the same rate, and the ventricular contractions should follow the atrial contractions. In this case however, the atrial contractions are much faster (123 beats per minute) than the ventricular contractions (47 beats per minute) and the atrial and ventricular contractions are completely unrelated. A normal fetal heart rate is about 140-150 beats per minute; this fetus's heart rate was only 47 beats per minute!
As many as 1/3 of fetuses with AV block die before birth or in the first year of life. Fetal AV block is almost exclusively associated with maternal anti-Ro/SSA or Sjogren's antibodies. While some women have symptoms of
autoimmune diseases
(e.g. like
Lupus
or
Sjogren's syndrome),
the mothers of about 50% of fetuses with heart block are not aware they carry the antibodies (anti-Ro/SSA) until the fetus is diagnosed. Although fetal AV block is relatively rare in the overall population (about 1,000 babies in the U.S. each year), its high mortality rate means that fetal heart block is an issue of great concern for mothers with anti-Ro/SSA antibodies and the doctors who care for them.
Dr. Henry Galan is a maternal fetal medicine specialist at the Colorado Fetal Care Center at Children's Hospital Colorado who cares for mothers with high risk pregnancies including those anti-Ro/SSA antibody positive mothers, and mothers whose fetuses develop fetal AV block. Fetal AV block is also of great concern for Dr. Bettina Cuneo, a pediatric and fetal cardiologist at the Colorado Fetal Care Center at Children's Hospital Colorado. Dr. Cuneo continues to push the boundaries of medicine to diagnose and treat early forms of fetal AV block before it is irreversible. Most recently, Dr. Cuneo and a team of specialists at the Colorado Fetal Care Center adopted a method called the EXIT (ex-utero intrapartum treatment) to deliver a premature fetus with AV block and heart failure. This baby is now one year old, and with the careful attention of cardiologists, is expected to live a long, happy life.
The Fetal Heart
The fetal heart begins to develop immediately following conception, and by about eight weeks of gestation the structures of the heart are fully formed. These structures include the
right atrium
and
left atrium,
which receive blood, and the
right ventricle
and
left ventricle,
which pump blood. Circulating blood flows from the body into the right atrium to the right ventricle, where it is pumped into blood vessels that pass through the lungs, allowing for gas exchange and the blood to become oxygenated. The newly oxygenated blood then flows into the left atrium to the left ventricle and is pumped out to the rest of the body.
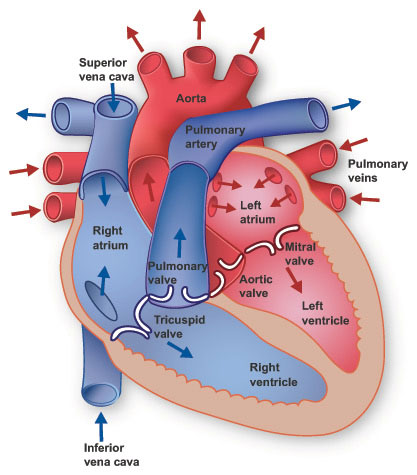
Figure 2. Picture of the human heart.
[Source: https://www.texasheart.org/heart-health/heart-information-center/topics/heart-anatomy/]
The rate of blood flowing through the heart is controlled by two nodes: the
sinoatrial node
and the
atrioventricular node.
Both nodes are made of bundles of fibers of nervous tissue that control the firing of heart cells and maintain our heartbeat. The sinoatrial node receives messages from the
autonomic nervous system
to allow blood into the atria, making it possible for the heart to beat. The sinoatrial node sends messages to the atrioventricular node, which allows the ventricles to contract, producing the actual heartbeat.
Fetal AV Block
Fetal AV block occurs when the anti-Ro/SSA antibodies cross the
placenta
and cause inflammation and
fibrosis
of the fetal AV node and the heart muscle itself. The anti-Ro/SSA antibodies are present in about 3% of all women and are commonly associated with autoimmune disorders including systemic lupus, Sjogren's syndrome and related autoimmune diseases. In mothers with anti-Ro/SSA antibodies, approximately 2 to 4% of fetuses will develop AV block.
Fetal AV block can be divided into three stages based on the damage done to the atrioventricular node: first degree, second degree, and third degree. The degrees refer to the transmission time of the electrical signals from the sinoatrial node to the atrioventricular node. In first degree heart block, the transmission is delayed; by third degree heart block, no electrical signals are being transmitted. The inability of the heart to beat results in a buildup of blood waiting to get into the lungs and then out into the body. The failure of the heart to beat can cause irreversible damage to the fetal heart tissue and other organs. In the case of fetal heart block, time is of critical importance, because the fetus can develop first degree heart block that leads to permanent third-degree damage in under 24 hours. However, if the fetus receives proper treatment (delivered through the mother), first and second-degree heart block can be reversed, avoiding permanent, life-altering damage. The fetus cared for by Dr. Galan and Dr. Cuneo already was in irreversible 3rd degree AV block.
a.
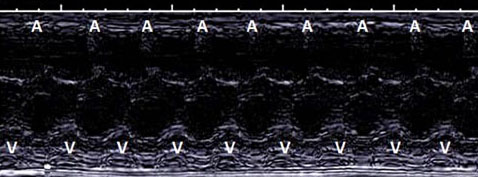
b.
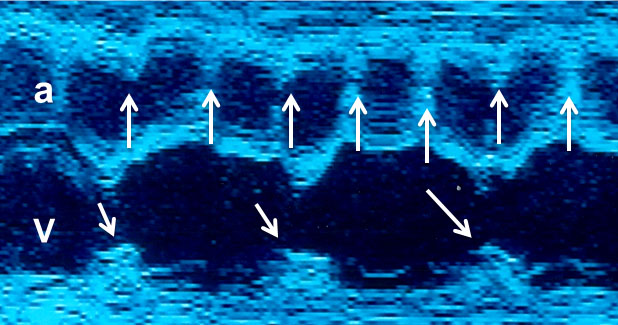
Figure 3a. M-mode of normal rhythm and b. M-mode of complete AV block
Fetal Heart Block Prevention and Treatment
Dr. Cuneo and her colleagues have developed a unique surveillance technique for fetuses with irregular heartbeats at risk of developing fetal AV block. In a study called
"Heart Sounds at Home,"
Dr. Cuneo and her colleagues gave pregnant anti-SSA/Ro mothers commercial, FDA approved fetal heart rate monitors with instructions to monitor their developing baby's heart rate twice daily. The mothers monitored the fetal heart rates during the period of greatest risk for AV block: 18-25 weeks. They also had fetal echocardiograms every other week, which is the standard of care for fetal AV block surveillance. If the mothers measured an irregular heartbeat at any time during the study, they were instructed to come to the hospital for further evaluation. By mothers detecting the first abnormal heart beat and physicians diagnosing the irregular rhythm as 2nd degree AV block, prompt treatment restored normal rhythm. Not only were the mothers able to deliver normally (as opposed to a cesarean or
c-section
which is needed for delivering fetuses with 3rd degree AV block), but the babies have not needed pacemakers in the first years of life. The study was very successful, and Dr. Cuneo is now submitting an international clinical trial grant with rheumatologist Dr. Jill Buyon from New York University in New York City using commercial fetal heart rate monitors to detect 2nd degree AV block. The purpose of the study is to determine the best treatment to restore normal heart rhythm.
In addition, Dr. Cuneo assists mothers who are unable to get to the Colorado Fetal Care Center for their surveillance fetal echocardiograms through a telemedicine program. Since fetal cardiology is a rare specialty, it is not always available at local hospitals where mothers go to get prenatal care. The telemedicine program allows Dr. Cuneo to attend medical appointments and review echocardiograms done remotely. In this way, Dr. Cuneo can assist patients all over the country.

Figure 4. Dr. Cuneo conducting a telemedicine appointment.
Unfortunately, even with this improved care, not all cases of fetal AV block are detected early enough to treat. Once a baby develops 3rd degree AV block, the goal is to keep the baby in the womb as long as possible without developing heart failure.
Even if doctors can treat the mother and fetus successfully until the time of birth, delivery presents its own complications. Once the fetus is removed from the womb, it no longer has the mother's support. When the umbilical cord is cut, the normal baby's heart rate increases to meet the demands of birth. A newborn with AV block cannot increase their heart rate. To give these babies the greatest chance of survival, Dr. Cuneo coordinated with a team of colleagues to surgically implant a
pacemaker
in the newborn baby immediately following birth. As the mother was giving birth in one room, the neonatal surgical team was waiting in the room next door. The pacemaker was in place only 20-30 minutes following birth.
But it wasn't enough. Twice, Dr. Cuneo and her team lost newborn babies when their systems were overwhelmed before the pacemaker was in place, unable to survive past the delivery room. Determined not to lose another baby this way, Dr. Cuneo and her colleagues worked to develop an alternative treatment that would decrease the time the newborn was in the world without cardiac support. They settled on a treatment plan called
ex utero intrapartum treatment
or EXIT procedure. "Intrapartum" means that the surgery would occur literally during birth. The EXIT procedure is used for babies who cannot breathe after birth without surgery. This is the first time the EXIT procedure was adapted for delivery of a fetus with fetal AV block.
Helping Fetuses EXIT the Womb
The fetus that would become the first to undergo this procedure had developed complete AV block at 19 weeks of gestation due to maternal anti-Ro/SSA antibodies, which were previously undiagnosed in the mother. By 36 weeks, despite medications to augment the fetal heart rate, the heart rate had dropped dangerously low. Dr. Cuneo and Dr. Galan decided it was time to deliver the baby.
In addition to Dr. Cuneo and Dr. Galan, the Colorado Fetal Care Center doctors and healthcare team in the delivery room represented a range of specialties including,
neonatology
(Dr. Regina Reynolds and Dr. John Kinsella), fetal surgery (Dr. Rony Marwan and Dr. Tim Crombleholme), cardiac electrophysiology (Dr. Johannes von Alvensleben), and cardiothoracic surgery (Dr. Max Mitchell). The mother was put under general anesthesia as the cesarean delivery was performed. An incision was made in the mother's uterus and the baby entered the world—but only half way. This was part one of the delivery.
With the newborn baby's head and shoulders exposed, the team placed a tube into the baby's throat to assist with breathing and an intravenous line into the arm to deliver medications. Then the surgeons surgically attached temporary pacing wires directly to the newborn's right ventricle. During this time, the newborn was still attached to its mother through the umbilical cord to maintain the flow of blood and nutrients. Fifty-five minutes after the baby was exposed and with the heart rate increased by the pacemaker, the newborn was fully delivered, and the umbilical cord cut.
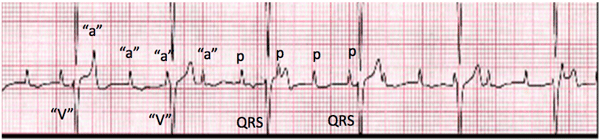
Figure 5. The heart rhythm tracing of a newborn with complete AV block. The "a"- waves we saw on the M-mode echocardiogram correspond to the p-waves on the rhythm tracing and the "v"-waves correspond to the QRS complexes.
The newborn stayed in the neonatal intensive care unit for several days to receive constant monitoring of heart rate and function. After three days, Dr. Mitchell removed the temporary pacing leads and implanted a permanent cardiac pacemaker. Today the twice-delivered baby is a year old and thriving. This child will need life-long monitoring by cardiologists, and the pacemaker will need to be changed as the child grows. Most importantly, though, the child is alive—thanks to the ingenuity of a stellar interdisciplinary team.
Future EXITs
Ex utero Intrapartum Treatment is not for everyone. In fact, Dr. Cuneo would only recommend the procedure in extreme cases: fetuses with low heart rates and heart block who are unlikely to survive any other way. The EXIT procedure is not without risks, since the mother must undergo general anesthesia and there is a risk of the mother losing too much blood.
In the future, Dr. Cuneo hopes to develop better treatments to detect heart block earlier and reverse the condition, so that no more babies need to be born through EXIT due to heart problems. "I don't believe any baby should be born with heart block," concludes Dr. Cuneo. "That's my ultimate goal."
Dr. Cuneo understands that performing the EXIT procedure was risky. But Dr. Cuneo wanted to try to make sure the baby would live—and she was willing to put her reputation on the line—and, as a result, a high-risk fetus with heart block is now a healthy one year old. "The most important thing is to learn from treatments that didn't work and move forward-even if it has never been done and failure is a possibility. It is a great gift to work with a team that looks for solutions outside the box, and whose goal is to give every person the opportunity to become a parent," explains Dr. Cuneo.
Dr. Bettina Cuneo is Professor of Pediatrics and Obstetrics, and Director of Perinatal Cardiology and Fetal Cardiac Telemedicine at Children's Hospital Colorado in Aurora, Colorado. Dr. Cuneo was always interested in cardiology and pediatrics, and she continues to work at the forefront of this new subspecialty of fetal cardiology. When not seeing patients, Dr. Cuneo enjoys spending time with her three children and cycling Gran Fondos and century rides.
Dr. Henry Galan is Professor of Maternal Fetal Medicine at the Colorado Fetal Care Center at the University of Colorado School of Medicine. When not seeing patients, Dr. Galan enjoys exercising, spending time with his family and his dogs-a yellow lab, a German shorthair pointer and a Havanese.
For More Information:
- Cuneo, B. et al. 2017. "Ex utero Intrapartum Treatment to Ventricular Pacing: A Novel Delivery Strategy for Complete Atrioventricular Block with Severe Bradycardia." Fetal Diagnosis and Therapy, 42(4): 311-314.
- Cuneo, B. et al. 2016. "Heart sounds at home: feasibility of an ambulatory fetal heart rhythm surveillance program for anti-SSA-positive pregnancies." Journal of Perinatology, 37(3): 226-230.
- Cuneo, B. et al. 2010. "A management strategy for fetal immune-mediated atrioventricular block." Journal of Maternal-Fetal & Neonatal Medicine, 23(12): 1400-1405.
- Zhao, H. et al. 2008. "Electrophysiological Characteristics of Fetal Atrioventricular Block." Journal of the American College of Cardiology, 51(1): 77-84.
To Learn More:
- Colorado Fetal Care Center. https://www.childrenscolorado.org/doctors-and-departments/departments/colorado-fetal-care-center/
- Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/heartdefects/index.html
- American Heart Association. http://www.heart.org/HEARTORG/Conditions/CongenitalHeartDefects/Congenital-Heart-Defects_UCM_001090_SubHomePage.jsp
Written by Rebecca Kranz with Andrea Gwosdow, PhD at www.gwosdow.com
HOME | ABOUT | ARCHIVES | TEACHERS | LINKS | CONTACT
All content on this site is © Massachusetts
Society for Medical Research or others. Please read our copyright
statement — it is important. |

