| |
According to the United States Fire Administration,
the risk of dying in a home fire is cut in half in homes with a working smoke alarm.
Indeed, the home smoke detector was listed as one of the
100 all-time gadgets by TIME magazine in 2010.
There are several types of smoke detectors using different mechanisms, but the basic concept is the same: early detection leads to smaller fires and saves lives. New work by a collaborative team of engineers, researchers and clinicians uses the same concept as the smoke detector to address a different type of fire: the surge of electrical energy in the brain that occurs during a
seizure.
In October 2014, What A Year! featured Drs. Chris Dulla and David Cantu of Tufts University who study the development of recurring seizures, a disorder known as
epilepsy.
Recall that
epilepsy
usually develops as a result of brain injury such as infection, tumor,
stroke
or
traumatic brain injury.
The time between initial injury and first seizure may range from a few days to many years, and there may be no other symptoms during this time. As Drs. Dulla and Cantu are finding, though, there are significant changes in the brain that may precede the behavioral symptoms of epilepsy.
This month we also focus on epilepsy, shifting from the origins of epilepsy to the management of the disease. The Centers for Disease Control and Prevention estimate that epilepsy affects about 2.2 million adults and nearly 500,000 children in the United States. Epilepsy is a chronic condition, meaning that once it develops it cannot be cured. About 70% of people with epilepsy successfully manage the condition with medication. There are a variety of medications available that help reduce the frequency and severity of seizures. Alternative treatments such as specific diets can also be used to control epilepsy in some patients. For patients who do not respond to medication or diet management, brain surgery to remove parts of the brain or implant small devices is sometimes considered.
Controlling epilepsy is important because seizures can be dangerous. Seizures are caused by surges in electrical activity that occur when normal brain regulation is disrupted. In extreme cases, seizures can lead to irreversible brain damage or even death.
Seizures are caused by surges in electrical activity that occur when normal brain regulation is disrupted. These changes in brain activity can be localized - known as a partial seizure - or can occur in many different parts of the brain simultaneously - known as a
grand mal seizure.
A seizure can occur at any time of the day or night, and the timing of such events is difficult or impossible to predict. The symptoms and severity of a seizure depend on the part of the brain affected. A seizure can be a mild, localized event where the person becomes unable to move for a few moments and then returns to normal again. A seizure can also involve severe thrashing and unconsciousness. In extreme cases, seizures can lead to irreversible brain damage or even death.
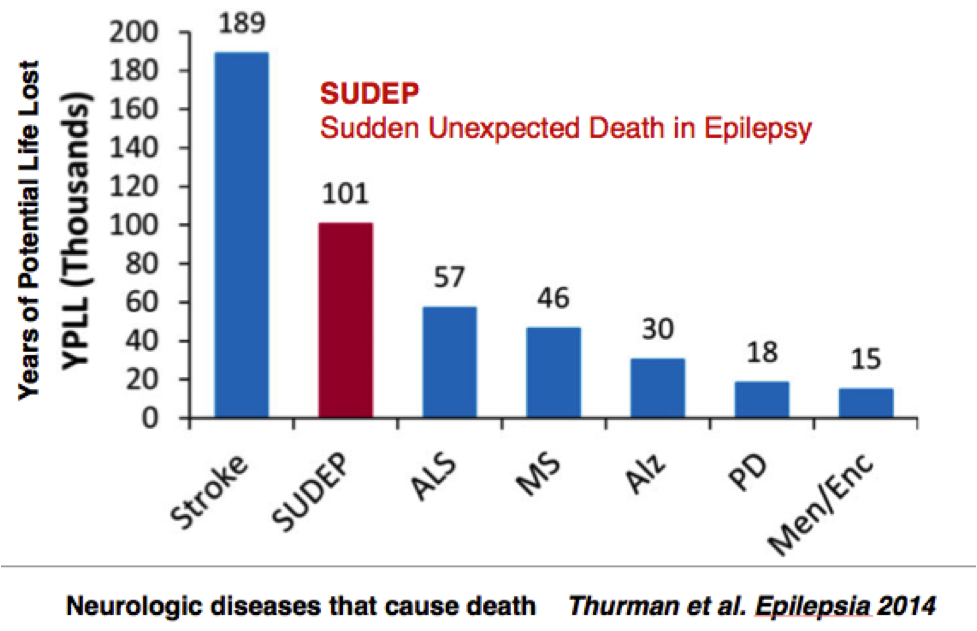
Sudden Unexpected Death in Epilepsy
The most common cause of death for people with epilepsy is known as
sudden unexpected death in epilepsy
or SUDEP for short. SUDEP refers to the death of a person with epilepsy that happens unexpectedly for no clear cause. In most cases, the person has died during sleep. From monitored cases (where the patient died while wearing an
electroencephalogram
or EEG monitor with video observation), the cause was that he or she stopped breathing at some point during or after the seizure, and then later
the heart stopped.
SUDEP is important because it causes more years of life lost among neurological diseases than amyotrophic lateralsclerosis (ALS) [Lou Gehrig's disease], Parkinson's disease (PD), multiple sclerosis (MS), Alzheimer's disease, and meningitis/encephalitis (Men/Enc),
as indicated in the figure below.
According to the Epilepsy Foundation,
SUDEP occurs in one of every thousand epilepsy patients each year.
Patients with uncontrolled seizures have a higher risk of SUDEP.
"There is a very simple way that may prevent many cases of SUDEP," explains Dr. Rosalind Picard, Professor, and Director of Affective Computing Research at Massachusetts Institute of Technology. "If you would simply stimulate the person, then they may start breathing again. By waking up the person, or perhaps even just turning them over, you might save his or her life."
Of course, this simple solution is actually quite complex. In order for someone to be able to "simply" wake you up after a seizure, they have to be physically close enough to you to know that you have had a seizure. Dr. Picard describes a sixteen-year-old student with epilepsy who still sleeps in the same bed with her parents to prevent SUDEP or other nighttime seizure-related complications. Some adults with epilepsy have no choice but to live alone; many adults fear never waking up after a nighttime seizure.
"This is a serious problem," Dr. Picard comments. "More people die from SUDEP than from house fires."
To address the problem of people dying from SUDEP, Dr. Picard developed a device that would act as a "smoke detector" for seizure activity.
This device was not originally intended to be used for patients with epilepsy. At the time the project began, Dr. Picard was studying ways that technology can sense, model, and respond to emotion. Her research team had developed a sensor to measure emotional stress in children with
autism.
Many people with autism show emotions differently on the outside, and this can cause them to be very misunderstood. Picard hoped that the device could provide insight for parents and caregivers about why their child was upset, and help them see how to make accommodations to reduce stress for the child.
Serendipity
An undergraduate student at the time asked Dr. Picard to borrow the device to test on his younger brother with autism over winter break. Dr. Picard gave the student two sensors. "I told him to use one and keep the other as a back-up in case the first broke, since they were built by hand and fragile back then. It's a good thing he didn't listen to me." Instead of doing as Dr. Picard had instructed, the student placed both sensors on his brother at the same time, one on the right wrist and one on the left.
Dr. Picard was looking at the data on her laptop at MIT. The devices seemed to be working properly until she came across one very abnormal piece of data. At one point in time, one of the sensors indicated a dramatic stress response while the other sensor - on the opposite side of the body - did not. "I could not figure out what was going on. I thought one or both of the sensors must be broken," Dr. Picard recalls. Unable to make sense of the data, Dr. Picard called the student during vacation. She asked what the student's brother had been doing on the day and time of the abnormal recording. Referring to his brother's daily log, the student reported that the time was twenty minutes before his brother had a seizure.
At the time, Dr. Picard knew nothing about seizures. "I had to start doing some research," she recalls. Dr. Picard began by contacting a student's father, a
neurologist
and brain surgeon at Boston Children's Hospital, Dr. Joe Madsen. Dr. Madsen explained that a seizure could affect just one side of the body, and he became interested in learning more. They set up an experiment to get more data.
Building a Better Sensor
MIT graduate student Ming-Zher Poh redesigned the wrist sensor to reliably record data and motion at a high resolution. Poh worked with Dr. Tobias Loddenkemper, a pediatric neurologist at Boston Children's Hospital who specializes in epilepsy, to design and carry out studies on children with epilepsy, who were in the hospital being monitored. The main signals measured by the device were motion and electrical changes on the surface of the skin, known as
electrodermal activity.
The data were processed by an onboard data chip powered by a small lithium battery and stored on a memory card.
How are changes on the skin related to nerve activity? All embryos are composed of three tissue types: the
endoderm,
mesoderm
and
ectoderm.
All of the tissues in our bodies are derived from just these three tissue types. The
gastrointestinal tract,
liver
and
pancreas
are derived from the endoderm; the mesoderm forms muscles including skeletal, smooth, and heart tissue, connective tissues and the
kidneys;
both skin and the
nervous system
are derived from the ectoderm. The skin and nervous system are connected because they are derived from the same type of tissue.
Having identified a potentially novel purpose for the sensor, Drs. Picard and Loddenkemper worked together with Poh to make the technology available for patients. Dr. Loddenkemper received hospital approval and permission from 80 patients to test the sensor when they came to the hospital for scheduled visits. These patients were admitted to the long-term video-electroencephalogram monitoring unit. As mentioned above, the
electroencephalogram,
or EEG for short, is a test that measures electrical activity in the brain by attaching
electrodes
to the scalp. Electroencephalograms help doctors understand what parts of the brain are affected during seizures. "This is incredibly valuable information that helps doctors better treat their patients with epilepsy," Dr. Loddenkemper explains. Patients who agreed to wear the sensor developed in Dr. Picard's laboratory would simultaneously undergo EEGs and video monitoring. This allowed the researchers to compare data from the sensor with data obtained through the EEG and video recordings.
In over 4,000 hours of recordings obtained from 80 patients, the sensor detected 15 of 16 grand mal seizures with an average of less than one false alarm a day. Dr. Picard and Ming-Zher Poh used a complex mathematical process known as
machine learning
to analyze the data. The goal was to find equations or formulas that led to the observed results. As the researchers gathered more and more data, they were able to create better computer models that more accurately identified seizure activity. For example, some of the false positives the sensor identified occurred when the patients were waving their arms and making large movements while playing video games. Better mathematical modeling leads to more precise algorithms, and a more accurate sensor.
The researchers also learned something else surprising: the size of the response the wrist sensor records is highly correlated with a key biomarker present in SUDEP.
The researchers also learned something else surprising: the size of the response the wrist sensor records is highly correlated with a key biomarker present in SUDEP. They published their findings - the seizure detection algorithm, and the connection to SUDEP, in two top medical journals.
Making a Marketable Product
Given the success of the findings in the hospital, Dr. Picard tried to get her company Affectiva, Inc to take them to market. When that attempt failed, she started another company, merged it with an Italian company, and formed Empatica, Inc, which is now delivering the sensor patients will need. In the laboratory, patients are wearing the sensor indoors for limited amounts of time. A device for patients to bring home, on the other hand, would need to be comfortable enough to be worn all day and robust enough to function while doing the normal daily activities of the people wearing them. It would also need to look cool and perform functions that were not limited to medical uses, so that it would not be stigmatizing.

Embrace wristband
The device developed by Empatica, Inc has two parts: the device itself, called
Embrace,
and a buddy device - a smartphone or tablet. Similar to the one developed for the hospital study, Embrace measures temperature, motion, and electrodermal activity. From these, a patient can get logs of sleep, physical activity, seizures and autonomic stress. The data are instantly processed within the device using custom algorithms developed to detect patterns of seizure activity. If the data patterns of the person wearing the Embrace match the pattern of a seizure, then Embrace will activate an alarm. The wearer gets a gentle vibration and notification, and if they don't cancel it, then the alarm is sent wirelessly, through the smartphone or tablet, to one or more caregivers whom the patient has designated. They will get an alert with a phone call or
short message service (SMS)
asking them to check on the patient. Doctors can provide specific instructions to accompany the alert. For example, they may recommend to give a medication or simply to stimulate the person by turning them over to make sure they are breathing. Normal human intervention may sometimes be all the person with epilepsy needs to wake up the next morning. "It's been a long process," says Dr. Picard. "But it was certainly worth it. This technology will save lives."
Embrace is set to be released to people who pre-ordered it on Indiegogo in the Summer of 2015, and for commercial use in Fall 2015.
Dr. Rosalind Picard is Professor of Media Arts and Sciences at the Massachusetts Institute of Technology (MIT) Media Laboratory in Boston, MA. She is the Founder and Director of the Affective Computing Research Group at MIT. In fact, Picard coined the term "affective computing" to refer to her field of research, focusing on how technologies communicate, model, and respond to emotion. Dr. Picard has founded two companies: Empatica, Inc. to develop wearable sensors and Affectiva, Inc. developing technologies to measure emotion. When she's not in the laboratory, Dr. Picard enjoys playing tennis, biking, gardening, shopping, and spending time with her family.
Dr. Tobias Loddenkemper is a Pediatric Neurologist at Boston Children's Hospital specializing in children with epilepsy and Associate Professor of Neurology at Harvard Medical School. He regularly sees patients and also participates in a variety of research projects to improve patient care. When not in the laboratory, Dr. Loddenkemper enjoys hiking, biking, and spending time with his family.
Dr. Ming-Zher Poh was a graduate student at MIT in Dr. Picard's laboratory while developing the technology for the sensor, which was his Ph.D. research. "He's the one who really took this project on and moved it forward," remarks Dr. Picard. Dr. Ming has since graduated and founded his own company called Cardiio based on another project he developed in graduate school. He continues to improve methods for detection of epileptic seizures as a Research Affiliate at the MIT Media Lab.
For More Information:
- Poh, Ming-Zher et al. 2012. "Convulsive seizure detection using a wrist-worn electrodermal activity and accelerometry biosensor." Epilepsia, 53(5): e93-d97.
- Poh, MZ et al. 2010. "Continuous monitoring of electrodermal activity during epileptic seizures using a wearable sensor." Conf Proc IEEE Eng Med Biol Soc. 2010:4415-8.
- Poh, MZ et al. 2012. Autonomic changes with seizures correlate with postictal EEG suppression. Neurology. 5;78(23):1868-76.
To Learn More:
Epilepsy
- Epilepsy Foundation. http://www.epilepsy.com/
- National Institute of Neurological Disorders and Stroke. http://www.ninds.nih.gov/disorders/epilepsy/epilepsy.htm
- Wristband Could Predict Severe Epileptic Seizures. http://www.huffingtonpost.co.uk/2012/04/27/wristband-predict-epileptic-seizures_n_1458294.html
Wearable Technology
- Affective Computing Media Lab. http://affect.media.mit.edu
- Empatica, Inc. http://www.empatica.com
- Affectiva, Inc. http://www.affectiva.com
- Cardiio, Inc. http://www.cardiio.com
Written by Rebecca Kranz with Andrea Gwosdow, PhD at www.gwosdow.com
HOME | ABOUT | ARCHIVES | TEACHERS | LINKS | CONTACT
All content on this site is © Massachusetts
Society for Medical Research or others. Please read our copyright
statement — it is important. |
|
|

Dr. Tobias Loddenkemper
(Photo by Katherine C. Cohen/Boston Children's Hospital)

Dr. Rosalind Picard
Dr. Ming-Zher Poh
Sign Up for our Monthly Announcement!
...or  subscribe to all of our stories! subscribe to all of our stories!

What A Year! is a project of the Massachusetts
Society for Medical Research.
|
|

