| |
Did you know that you spend about one-third of your life asleep? While all of the biological functions of sleep are still not fully known, we do know that sleep is absolutely necessary for good health.
People who do not get enough sleep find it hard to focus, or they may find themselves dozing during class or on the job. There are many reasons you may not get enough sleep on a particular night or during a particular week: too much work, a mid-night phone call, another TV episode you just had to see. Some people periodically or regularly suffer from insomnia, a condition in which it is difficult to fall or remain asleep. And some people suffer from the serious sleep disorder called narcolepsy, a lack of prolonged sleep that can have severe consequences.
It is estimated that around one person out of every thousand is affected by narcolepsy. One of the characteristics of narcolepsy may be sleep paralysis. Your body becomes paralyzed while you are dreaming because, if it didn’t, you would act out your dreams and it could be very dangerous. Narcoleptics may have vivid dreams and sleep paralysis, in which the body is still paralyzed even after awakening from a dream. The condition can last for several minutes, just before falling asleep or just after waking up. This is quite scary to people who experience it: imagine what it would be like to be awake and unable to move!
Another possible distinguishing characteristic of narcolepsy is cataplexy. Cataplexy refers to muscle collapse due to an emotional stimulus such as becoming very happy or very angry. As our friends at Stanford University note, cataplexy is “a striking, sudden episode of muscle weakness triggered by emotions. Typically, the patient's knees buckle and may give way upon laughing, elation, surprise or anger. In other typical cataplectic attacks the head may drop or the jaw may become slack. In severe cases, the patient might fall down and become completely paralyzed for a few seconds to several minutes.” Not all narcoleptics experience cataplexy.
Narcoleptics also typically suffer from excessive daytime sleepiness and difficulty sleeping at night. Life for people with narcolepsy can be very difficult. Sporadic napping or bouts of cataplexy can make finding a job or leading a normal social life very tough. To get a sense of how difficult, painful and even scary life with narcolepsy can be, spend three minutes with this YouTube video: http://www.youtube.com/watch?v=3MBCeKn0Oeo
Old School Treatments
When Dr. Emmanuel Mignot of the Stanford University School of Medicine first began studying narcolepsy, the treatment options for patients were rather slim. First of all, the time between the onset and diagnosis of narcolepsy in a patient averaged around fourteen years. There were most likely many narcoleptics who died without ever knowing what they had suffered from. Treatments for the disease include anti-depressants to suppress cataplexy, amphetamines to stay awake and sleep medications to induce sleep. Many narcoleptics became addicted to sleep medicines and the medications did not work well. Two decades later, the time between the onset and diagnosis of narcolepsy has been reduced to an average of three years, and there are many more treatment options. The leap in our understanding of narcolepsy has been in large part due to his research.
Dr. Mignot completed his medical training in Pharmacology and Psychiatry in France before coming to the United States. He had decided to focus his attention on sleep because it was such a basic phenomenon, and the unique symptoms of narcolepsy demanded his attention. As a physician scientist, he was surprised to find that very few researchers were studying such an interesting disease.
As a pharmacologist, Dr. Mignot first began by developing better treatments for narcolepsy. He was rapidly joined by Dr. Seiji Nishino, a Psychiatrist from Japan. Together, they made some improvements in treatment, and became interested in studying the genetics of the disease. This was possible because another Stanford researcher, Dr. William Dement, had discovered narcolepsy in dogs and found that the canine form of the disease was genetic.
The Stanford team then used this dog model of narcolepsy to search for the gene for canine narcolepsy. It took Dr. Mignot and his research team, Dr. Ling Lin and Dr. Juliette Faraco, ten years. Eventually they were successful in locating the cause of canine narcolepsy: a disruption in the hypocretin receptor 2 gene, or Hcrtr2.
Dr. Mignot’s findings implicated the group of proteins known as the hypocretins as the cause of narcolepsy in dogs. Hypocretin is a very small protein, also called a peptide, that is produced by neurons in a part of the brain called the hypothalamus. Dr. Mignot wondered if this same protein was involved in narcolepsy in humans.
Missing in Dogs, Missing in Humans
When Dr. Mignot looked for hypocretin in humans with narcolepsy, he found the protein was missing. He hypothesized there were two possibilities for this lack of hypocretin in people with narcolepsy: either (a) the cells died off, or (b) the protein was not produced in the first place. If the cells died, this could suggest that an autoimmune process was involved. An autoimmune process occurs when your own immune system mistakes healthy cells in your body for abnormal cells. This sets off an immune response that attacks and destroys healthy cells. Any time your own body is destroying its own healthy cells, there is likely to be problem.
A Genetic Association Study
To determine if there was some genetic basis for this lack of hypocretin in human narcolepsy, Drs. Mignot, Joachim Hallmayer, Faraco at Stanford, and collaborators at UCSF, Dr. Neil Risch and Dr. Pui Kwock, conducted a series of genetic association studies with the help of numerous clinical sleep researchers. Genes are encoded, or “written”, using four nucleotides that can combine in an almost infinite number of ways. This is what makes each human being unique on the genetic level. Using new technologies, it is now possible to determine the sequences of nucleotides for every single gene in your body from a blood sample. A genetic association study compares the sequences of nucleotides between individuals.
Now, a comparison of just two individual sequences would not be too insightful because there would be thousands and thousands of differences. There would be no way to tell if one particular difference was meaningful. For this reason Dr. Mignot and colleagues used blood samples from two thousand people for his study – one thousand samples from people with narcolepsy and one thousand samples from people without narcolepsy. They compared the sequences of each group of individuals. Their goal was to determine if there was a common genetic link in the narcolepsy patients that was different from the normal patients. They reasoned that such a link might indicate a genetic cause for the lack of hypocretin in narcolepsy patients. Dr. Mignot and his colleagues found two genes that were different in narcolepsy patients: the Human Leukocyte Antigen (HLA) gene and the T-cell receptor (TCR) gene. The HLA gene encodes for a protein that is very important in the immune response. The TCR gene is stimulated when T-cells bind to it, and induce an immune response. T-cells are a type of white blood cell vital to the immune response. These two genes are both very important in the immune response. This research provided solid evidence that the lack of hypocretin in narcolepsy patients involved the immune system.
The Immune System: Crucial But Not Fully Understood
The immune response to infection is a complicated process that is not completely understood. The immune response begins when an infectious agent such as a bacteria or virus invades the body. White blood cells recognize the pathogen and engulf it. Once engulfed, enzymes cut up the DNA or genetic material. A piece of the DNA is stuck to the cell membrane of white blood cells. If the piece of DNA matches the receptor, HLA is replicated and binds to TCR. This HLA-TCR complex8 is then available for an immune response. The exact process of how HLA-TCR complex results in disease is unknown.
Some of the Benefits of Sleep
- Learning and memory Sleep helps the brain commit new information to memory through a process called memory consolidation. In studies, people who’d slept after learning a task did better on tests later.
- Metabolism and weight Chronic sleep deprivation may cause weight gain by affecting the way our bodies process and store carbohydrates, and by altering levels of hormones that affect our appetite.
- Safety Sleep debt contributes to a greater tendency to fall asleep during the daytime. These lapses may cause falls and mistakes such as medical errors, air traffic mishaps, and road accidents.
- Mood Sleep loss may result in irritability, impatience, inability to concentrate, and moodiness. Too little sleep can also leave you too tired to do the things you like to do.
- Cardiovascular health Serious sleep disorders have been linked to hypertension, increased stress hormone levels, and irregular heartbeat.
- Disease Sleep deprivation alters immune function, including the activity of the body’s killer cells. Keeping up with sleep may also help fight cancer.
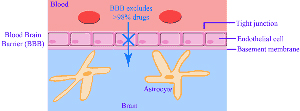
From Harvard Health Publications - https://www.health.harvard.edu/press_releases/importance_of_sleep_and_health.htm Once the hypocretin cells are destroyed, the body is left without any hypocretin and with the condition of narcolepsy. Dr. Mignot has identified a broad group of infectious agents he believes contributes to initiating the narcolepsy autoimmune response and is currently working on identifying the specific species involved. He also suspects that people with a head injury or high fever may be more susceptible to this autoimmune brain response because it would make it easier for the T-cells to cross the blood brain barrier.
What next?
One goal is to identify who is at risk for developing narcolepsy. Since narcolepsy in humans is dependent upon both genetics and the environment, people with the genetic changes in the HLA and TCR genes implicated in the genetic association study will not necessarily develop narcolepsy. And people who become infected with the infectious agent that causes narcolepsy will not necessarily develop the disease either. It is a combination of both of these factors.
Dr. Mignot plans to continue to further his research by looking more closely at the TCR-HLA complex. He would like to determine how exactly how that mechanism works. By understanding the mechanism, he hopes to develop a way to prevent narcolepsy, and eventually to find a cure as well.
Dr. Emmanuel Mignot is a Professor of Psychiatry and Behavioral Sciences and Director of the Center for Narcolepsy at the Stanford University School of Medicine. He received his medical and doctorate degrees in France before beginning his research career in the United States. Dr. Mignot’s research focuses on the cause and pathogenesis of narcolepsy; he is also a practicing physician who regularly sees patients with narcolepsy and other sleep problems. He has two sons and a narcoleptic dog he and his family adopted from his study on narcoleptic dogs. In his free time Dr. Mignot enjoys reading novels, traveling and spending time with his family.
To learn more:
- Mignot, E. and L. Lin. (2009) “Narcolepsy.” Encyclopedia of Neuroscience 6: 7-14.
- Mishima, Kazuo et al (2008). “Hypocretin Receptor Expression in Canine and Murine Narcolepsy Models and in Hypocretin-Ligand Deficient Human Narcolepsy.” Sleep 31(8) 1119-1126.
- Lin, L et al (1999). “The Sleep Disorder Canine Narcolepsy is Caused by a Mutation in the Hypocretin (Orexin) Receptor 2 Gene. Cell 98: 365-376.
For more information:
Written by Rebecca Kranz with Andrea
Gwosdow, Ph.D. Gwosdow
Associates
HOME | ABOUT | ARCHIVES | TEACHERS | LINKS | CONTACT
All content on this site is © Massachusetts
Society for Medical Research or others. Please read our copyright
statement — it is important. |
|
|

Dr. Emmanuel Mignot

Staff of the Center for Narcolepsy at Stanford University School of Medicine


Watch The Video
Short video of a little girl with narcolepsy. The video explains narcolepsy, sleep paralysis and cataplexy. The video is in English though the on-screen titles are not.
Video courtesy of YouTube.com
Sign Up for our Monthly Announcement!
...or  subscribe to all of our stories! subscribe to all of our stories!

What A Year! is a project of the Massachusetts
Society for Medical Research.
|
|

