| |
Highlights
Acupuncture is an ancient Chinese medicinal practice that can be helpful for patients with a variety of health conditions. Scientists do not yet fully understand how acupuncture works to reduce pain and inflammation. These researchers sought to use scientific understanding of the brain and nervous system to study the biological pathways that mediate the positive effects of acupuncture treatment. They showed that a select group of sensory neurons in the mouse hindlimb expressing a specific gene are necessary and sufficient to reduce inflammation in a mouse model of sepsis. In future studies, these researchers plan to apply their techniques to other disease types and organs. They also plan to conduct studies of acupuncture using human participants.
The Yangtze River is the largest river in Asia, beginning in the Tanggula Mountains of Tibet and flowing nearly 4,000 miles to the East China Sea.

Figure 1. Yangtze River, Yunnan Province, China
[Source: Jialiang Gao, https://simple.wikipedia.org/wiki/Yangtze_River#/media/File:Cn1202-03.jpg]
Along the way, there are hundreds of smaller rivers that feed into the large river. Certain areas along the river have seasonal flooding during the rainy season. “A big river with many smaller rivers that feed it is a useful metaphor for thinking about how our bodies experience pain,” commented Dr. Qiufu Ma, Professor of Neurobiology at Harvard Medical School and Dana Farber Cancer Institute who researches the biological mechanisms of pain. Since, from an evolutionary perspective, pain is so crucial to the survival of the human species, we have multiple pathways to send pain signals to the brain, like all the smaller waterways that feed the Yangtze River.
Dr. Ma began his career by studying the particular pathways that cause pain and
inflammation
in the body and how they become dysregulated. Along with many scientists in the field of pain research, Dr. Ma was looking for specific cell types or molecules that cause pain and inflammation. The goal was to identify specific targets that could be stimulated or blocked in order to reduce pain and inflammation in human patients. Over the past decades, researchers have identified many such therapeutic targets, but these targets have generally failed when tested in
animal models.
Several years ago, Dr. Ma began to shift the focus of his research. Rather than searching for precise molecules and pathways that cause pain and inflammation, he decided to try a different approach. As Dr. Ma sees it, searching for specific molecules within individual pain and inflammatory pathways is like trying to stop flooding by damming a single stream that feeds the river. It might be possible to stop the flow of a single stream, but it won’t stop the flood because water is pouring in from other streams and the rain that’s causing the flooding is still falling. “What we want to be able to do,” explained Dr. Ma, “is stop it from raining.”
Nerves, the Immune System, and Controlling Inflammation
In order to understand Dr. Ma’s research, let’s first learn about nerves, the
immune system,
and some common problems that occur when inflammatory pathways become dysregulated.
Inflammation is a critical evolutionary adaptation in response to injury or infection involving complex interactions among the immune system, a network of organs, tissues, and cells that work together to fight infection and heal wounds. The immune system and activated nerves cause swelling and inflammation due to the influx of cells and blood flow to the affected area. This influx leads to the release of pro-inflammatory proteins (called cytokines) made by some immune and non-immune cells. If all systems and pathways are healthy and working as they should, the swelling and inflammation will decrease once injured tissues start to heal or once infected viruses and bacteria have been killed, such that anti-inflammatory mechanisms start to take over.
However, like any system in the body, the pathways of inflammation can stop working like they should. For example, the often-deadly condition called
sepsis
occurs when an infection triggers an overreactive immune response. Strong immune reactions lead to the release of excessive pro-inflammatory cytokines. The excessive release of cytokines is called a “cytokine storm.” An overreactive immune response and cytokine storm can lead to damaged organs, organ failure, and death.
According to the Centers for Disease Control, 1.7 million adults in the United States develop sepsis each year, leading to an estimated 270,000 deaths. There are no effective treatments for sepsis because available anti-inflammatory remedies typically target only one inflammatory pathway. There are multiple inflammatory pathways and immune cells involved in sepsis, more than any single known treatment can address. Blocking individual cytokines is like damming individual small rivers again. What is needed is to stop the rain and flooding by targeting multiple anti-inflammatory pathways all at once. Similarly, following tissue or nerve injury, peripheral and central inflammation could fail to resolve, leading to the development of chronic pain and activation of many pain pathways.
While there are many ways that inflammatory pathways can become dysregulated, the body also has many internal mechanisms to resolve inflammation and to heal. Dr. Ma hypothesizes that if these healing pathways can be mobilized or enhanced, they could provide a way to treat dysregulated inflammatory disorders. To study this, Dr. Ma turned his research focus to acupuncture as a way to activate these anti-inflammatory pathways.
Acupuncture Research
Acupuncture is an ancient Chinese healing practice where thin needles are placed at specific points in the body. Acupuncture can be effective for patients with a variety of conditions including
chronic pain
and inflammation, persistent headaches and migraines, cancer, and side effects from cancer treatment, among others. Many patients who turn to acupuncture after receiving little help from
Western medicine
find the healing practice to be successful.

Figure 2. Acupuncture needles being placed by an acupuncturist
[Source: https://www.nccih.nih.gov/health/acupuncture-in-depth]
Dr. Ma decided to consider acupuncture for answers about inflammation control on a systemic level. He applied the techniques of Western science to better understand the underlying mechanisms that make acupuncture work. “Pain research over the past decades has identified many different signaling pathways involved in pain and inflammation,” explained Dr. Ma. “We now have the tools to understand from a scientific perspective how and why acupuncture works for some patients.”
Using Western scientific tools to better understand acupuncture is not new. Groundbreaking research conducted by Japanese researcher Akio Sato in the laboratory of Dr. Robert Schmidt in Berlin, Germany in the 1970s showed selective effects of acupuncture treatment at specific acupuncture points (acupoints) on the stimulated body region. Dr. Sato studied the process of how food moves through the digestive tract, known as
gastric motility.
When gastric motility is in balance, you can eat and go to the bathroom normally without pain or discomfort. However, too much gastric motility can lead to diarrhea and stomach cramps; too little gastric motility can lead to constipation and abdominal pain. Dr. Sato conducted studies on rats using needle pricks at specific acupoints all over the body to map their effects on gastric motility. He found that stimulating the hindlimbs of the rat at acupoint ST36 promoted gastric motility while stimulating the abdominal and chest region at acupoint ST25 inhibited gastric motility.
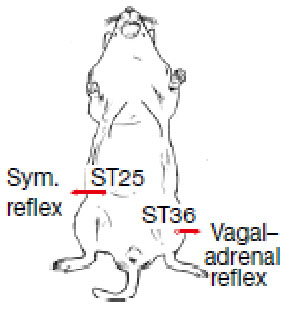
Figure 3. Location of acupuncture points ST25 on the abdomen and ST36 on the hindlimb
[Source: Liu et al. 2021, Figure 1a]
Moreover, when the associated nerves were blocked, this also blocked the effect of the acupoint stimulation. The nerve that mediated the effects of the hindlimb acupoint was the
vagus nerve.
The vagus nerve is the longest nerve of the
autonomic nervous system,
the part of the nervous system responsible for actions that are not consciously controlled. It is involved in many of our daily functions such as breathing, heart rate, and digestion, among others.
Several decades after Dr. Sato’s groundbreaking research, Dr. Bing Zhu, Professor and former President of the Institute of Acupuncture and
Moxibustion
in Beijing, China replicated Dr. Sato’s results using electrical stimulation rather than needle pricks. “This is such a fascinating puzzle for a neuroscientist,” commented Dr. Ma. “You have the exact same stimulation on different parts of the body, and you get drastically different results.” Dr. Ma visited Dr. Zhu in Beijing to learn his research techniques.
Dr. Ma used the research techniques he learned from Dr. Zhu to study how acupuncture works to reduce inflammation. Previous researchers such as Dr. Kevin Tracey, President, CEO, and Professor at the Feinstein Institutes for Medical Research and Dr. Luis Ulloa, Associate Professor of Anesthesiology at Duke University, had shown that stimulation of the vagus nerve could reduce systemic inflammation via a pathway known as the vagal-adrenal axis. Continuing this research, Dr. Ma and his team showed that the vagal-adrenal axis has regional specificity, similar to what Dr. Sato had found with gastric motility in the 1970s.
Dr. Ma used a mouse model of sepsis to see the effects of electrical stimulation at the same two acupoints, hindlimb region ST36 and abdominal region ST25, on systemic inflammation. He found that stimulation of the hindlimb region at acupoint ST36 reduced systemic inflammation, whereas stimulation of the abdominal region at acupoint ST25 had no effect. “These were interesting results,” recalled Dr. Ma, “but they didn’t answer our biggest question: why?”
The Why of Acupuncture
Dr. Ma hypothesized that there must be specific sensory pathways present in the limb region that were absent in the abdominal region. Such a difference would explain the observed regional specificity. Previous research identified a subset of
sensory neurons
in deep muscle tissue that showed developmental expression of the gene encoding the protein called prokineticin receptor 2 or PROKR2 was three to four times greater than in abdominal tissue. Dr. Ma wondered whether increased expression of PROKR2 in deep muscle tissue could explain why only stimulation of the limb region reduced inflammation.
This research was made possible by novel genetic techniques pioneered by some of Dr. Ma’s colleagues. Dr. Susan Dymecki developed a technique called intersectional genetics, which makes it possible for researchers to specify multiple properties of a cell to target. For example, Dr. Ma wanted to understand the function of PROKR2-expressing sensory neurons, but he faced the problem that PROKR2 is also expressed in many non-neuronal cells or in neurons located in other parts of the nervous system. Using the intersectional genetics strategy and genetic tools created in the laboratories of Drs. Martyn Goulding and David Ginty, Dr. Ma and his colleagues were able to create animals lacking only PROKR2-expressing sensory neurons.
Dr. Ma compared the effects of electrical stimulation of the hindlimb region in these experimental mouse models with controls. He found that without PROKR2-expressing sensory neurons that selectively innervate the hindlimb, electrical stimulation had no effect. This showed that these sensory neurons are necessary for electrical stimulation to produce an anti-inflammatory immune response.
Next, Dr. Ma used
optogenetics
to selectively activate only sensory neurons expressing PROKR2 in the hindlimb region. Optogenetics is a technique that uses light to activate specific cells.
By activating only PROKR2 sensory neurons in the hindlimb region, Dr. Ma was able to produce the same anti-inflammatory effect as electrical stimulation of the acupuncture point. This showed that PROKR2 neurons are the only cell type that need to be activated to produce this effect.
“This is an incredible result,” remarked Dr. Ma. “We have shown that, by stimulating this one area of the body, we can treat the flood, not by building small dams, but by actually stopping the rain.” In this case, the rain is the dysregulated immune response.
Dr. Ma has many plans for continuing this research. The methods used in this research can be applied to many other chronic diseases and organs. “We have identified just one of many anti-inflammatory pathways,” Dr. Ma commented. In addition, Dr. Ma hopes that research into the specific effects of acupuncture can be continued in studies with human subjects.
Dr. Qiufu Ma is Professor of Neurobiology at Harvard Medical School and Dana Farber Cancer Institute. His research focuses on mapping pain pathways and understanding the biological mechanisms of acupuncture.
To Learn More:
- Liu, S. et al. 2021. “A neuroanatomical basis for electroacupuncture to drive the vagal–adrenal axis.” Nature, 598: 641-5. https://www.nature.com/articles/s41586-021-04001-4
- Liu, S. et al. 2020. “Somatotopic Organization and Intensity Dependence in Driving Distinct NPY-Expressing Sympathetic Pathways by Electroacupuncture.” Neuron, 108(3): 436-50. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7666081/
- Borovikova, L. et al. 2000. “Vagus nerve stimulation attenuates the systemic inflammatory response to endotoxin.” Nature, 405: 458-62. https://www.nature.com/articles/35013070
- Kametani, H. et al. 1979. “Neural mechanisms of reflex facilitation and inhibition of gastric motility to stimulation of various skin areas in rats.” Journal of Physiology, 294: 407-18. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1280564/
To Learn More:
Acupuncture
- National Center for Complementary and Integrative Medicine.https://www.nccih.nih.gov/health/acupuncture-in-depth
- National Institutes of Health, News in Health.https://newsinhealth.nih.gov/2011/02/understanding-acupuncture
- Mayo Clinic.https://www.mayoclinic.org/tests-procedures/acupuncture/about/pac-20392763
Chronic Pain
- National Institute of Neurological Disorders and Stroke.https://www.ninds.nih.gov/Disorders/All-Disorders/Chronic-Pain-Information-Page
- Cleveland Clinic.https://my.clevelandclinic.org/health/diseases/4798-chronic-pain
- National Pain Advocacy Center.https://nationalpain.org/fast-facts-about-pain
Sepsis
- Centers for Disease Control and Prevention.https://www.cdc.gov/sepsis/what-is-sepsis.html
- National Institute of General Medical Sciences.https://www.nigms.nih.gov/education/fact-
sheets/Pages/sepsis.aspx
- Sepsis Alliance.https://www.sepsis.org/sepsis-basics/what-is-sepsis/
Written by Rebecca Kranz with Andrea Gwosdow, PhD at www.gwosdow.com
HOME | ABOUT | ARCHIVES | TEACHERS | LINKS | CONTACT
All content on this site is © Massachusetts
Society for Medical Research or others. Please read our copyright
statement — it is important. |
|
|

Dr. Qiufu Ma
Dr. Shen-Bin Liu

Dr. Zhi-Fu Wang

The Sugar Science Postcast
Episode 58: Qiufu Ma, PhD, Professor of Neurobiology at Harvard University, Dana-Farber Cancer Institute
Sign Up for our Monthly Announcement!
...or  subscribe to all of our stories! subscribe to all of our stories!

What A Year! is a project of the Massachusetts
Society for Medical Research.
|
|

