| |
The
year: 1982. The place: fast food restaurants in Michigan and Oregon.
The crime: sickening many and leaving 18 people dead. The culprit:
bacteria. Since 1983 outbreaks of Escherichia
coli (or E. coli for short) infections have
occurred sporadically throughout the United States. The one in
1982 was just the first. In 2006 and 2007, for example, dangerous
E. coli outbreaks have been traced back to spinach and
peanut butter. In between there have been dozens of reports of
illnesses and even deaths caused by E. coli infections.
Is this the result of an increase in the actual number of infections?
A new, more dangerous kind of E. coli? Or just better
reporting of what had been going on for years? What is all the
noise about?
Escherichia coli, a kind of bacteria,
are found in the intestinal tract of all mammals including humans.
They live in the lumen of the intestines and some even aid in
digestion. Normal E. coli are a necessary component in
digestion. But there is something different about the particular
E. coli strain that we are interested in this month. It is a
rare, dangerous strain of E. coli that doctors and researchers
have named O157:H7 (or sometimes just O157). There are two main
virulence factors that make this particular strain of E. coli
truly dangerous, pathogenic.
The first factor is the ability of E. coli O157:H7 to bind to the lining of the large intestine
without getting washed away. Other forms of non-pathogenic E. coli found normally in the gut get washed away by the material
flowing through the intestines. But E. coli O157:H7 have a surface protein called intimin that allow
them to attach more closely to the lining of the gut. The second
factor that makes E. coli O157:H7 so dangerous is its
ability to produce poisonous substances or toxins.
| The first sign of an E. coli O157 infection is bloody diarrhea. The bacteria cause damage to the lining of the large intestine and the toxins act on blood vessels in the gut, causing blood in watery stool or diarrhea. Once the lining has been broken down, the secreted toxins are more readily able to move through the intestinal lining and into the blood stream. These toxins are called shiga toxins (Stx). There are two types of shiga toxins: Stx1 and Stx2. Stx2 is more dangerous because, if taken up by the blood stream, it can cause kidney damage and eventual death in affected children or the elderly. The severe disease that these toxins induce is known as hemolytic uremic syndrome (HUS). |
 |
 |
 |
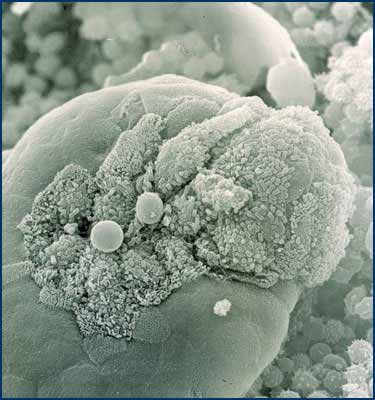
| Stx-producing STEC attached to the villi of the terminal ileum |
|
Dr. Saul Tzipori of the Tufts University
Cummings School of Veterinary Medicine has been studying diarrheic
diseases for over 30 years. Recently his team has developed a
treatment to protect patients against
HUS.
Dr. Tzipori and his team of researchers developed an antibody
that intercepts and binds to the toxin molecules in the blood
stream when it is given after the onset of diarrhea, but before
the onset of kidney failure. As a result, Stx2 is not taken up
by the cells in the kidney and other organs, preventing the development
of HUS. This antibody was derived in genetically modified mice
that are capable of making human antibody; it is extremely safe.
Dr. Tzipori’s novel idea is that this antibody targets the
toxins, not the bacteria itself. This means that the antibody
should work, even if the bacteria mutate. Therefore, the bacteria
cannot develop resistance against this treatment. The novel antibody
is now being developed into a drug.
Dr. Tzipori tested the drug in piglets and
mice. The piglet is an ideal model since it develops both phases
of the diseases: first diarrhea, which is followed by the effect
of the absorbed toxin through the damaged gut.
The drug will soon be tested in human adult
volunteers for safety and dose determination, known as Phase One
clinical trials. After testing in healthy adult volunteers it
will then be tested in additional (Phase Two and Phase Three)
clinical trials in sick children.
Where are you likely to meet E. coli?
It used to be that the most common way of
acquiring the bacteria was through undercooked meat. Cattle themselves are
the major host to this type of E. coli bacteria, even
though cattle show no signs of infection or contamination. This
makes the bacteria very hard to detect in them. The outbreaks
in 1982 were caused by undercooked meat at two McDonald’s
restaurants. “Since that time, fast food chains have found
that by cooking the meat more thoroughly under higher temperature,
they have eliminated this problem,” said Dr. Tzipori. One
way to avoid an unpleasant E. coli infection episode
is to cook your meat until it is well done. While this conflicts
with the way many people like their food, it is one sure method
for overcoming E. coli. Freezing does not kill E. coli bacteria of this strain; thorough cooking appears to
be the sole solution right now.
More recently, E. coli has been
spread through water contamination. “Cows produce lots of
fecal material,” said Dr. Tzipori, “which can make
its way into the rivers and streams. Likely the cause of contamination
of the spinach was irrigation using contaminated water.”
And for those of you who like to have something to worry about,
you can also be exposed to E. coli from unpasteurized
milk (or juice), raw sprouts and salami. If you swim in infected
pools or lakes or handle host animals and animal products, you
can also be infected. Deer and swine can carry the bacteria as
well.
|
|

The Microbiology and Botulism Research Unit.
Sign Up for our Monthly Announcement!
...or  subscribe to all of our stories! subscribe to all of our stories!

What A Year! is a project of the Massachusetts
Society for Medical Research.
|
|
| |
 Dr.
Tzipori is a Professor of Microbiology and Infectious Diseases and
Director of Infectious Disease at Tufts Cummings School of Veterinary
Medicine. Dr. Tzipori received his DVM and PhD from the University
of Queensland in Queensland, Australia. His dream was to become
a cow doctor, although things didn’t quite happen that way.
Bacterial diseases caused by E. coli are common amongst
animals, so Dr. Tzipori initially began studying the disease in
animals. He crossed over to human medicine once medical doctors
were convinced that E. coli diseases occurred in humans,
too. “The move was quite natural, actually,” said Dr.
Tzipori. “As to my credentials as a veterinarian working to
solve diseases of human health, 75 percent of infectious diseases
that have appeared in the last 50 years are zoonotic diseases.” Dr.
Tzipori is a Professor of Microbiology and Infectious Diseases and
Director of Infectious Disease at Tufts Cummings School of Veterinary
Medicine. Dr. Tzipori received his DVM and PhD from the University
of Queensland in Queensland, Australia. His dream was to become
a cow doctor, although things didn’t quite happen that way.
Bacterial diseases caused by E. coli are common amongst
animals, so Dr. Tzipori initially began studying the disease in
animals. He crossed over to human medicine once medical doctors
were convinced that E. coli diseases occurred in humans,
too. “The move was quite natural, actually,” said Dr.
Tzipori. “As to my credentials as a veterinarian working to
solve diseases of human health, 75 percent of infectious diseases
that have appeared in the last 50 years are zoonotic diseases.”
To Learn More:
- Tzipori, Saul, Abhineet Sheoran, Donna
Akiyoshi, Arthur Donohue-Rolfe, and Howard Trachtman. "Antibody
therapy in the management of shiga toxin-induced hemolytic
uremic syndrome." Clinical Microbiology Reviews. 17(2004):
926-941.
- Mukherjee , Jean, Kerry Chios, Dianne
Fishwild, Deborah Hudson, Susan O’Donnell, Stephen Rich,
Arthur Donohue-Rolfe, and Saul Tzipori. "Human stx2-specific
monoclonal antibodies prevent systemic complications of Escherichia
coli o157:H7 infection." Infection and Immunity 70(2002):
612-619.
- Muckerjee, Jean, Kerry Chios, Dianne
Fishwild, Deborah Hudson, Susan O’Donnell, Stephen Rich,
Arthur Donohue-Rolfe, and Saul Tzipori. "Production and
characterization of protective human antibodies against shiga
toxin 1." Infection and Immunity 70(2002): 5896-5899.
About E.Coli and the
Intestinal Tract:
- On NPR,
Deborah Franklin reports on the many little things living in
your gut and the risk of unbalancing them with improper use
of antibiotics. Click here
and then read the story or click the “Listen” icon.
Written by Rebecca Kranz with Andrea R. Gwosdow, PhD
Gwosdow Associates
HOME | ABOUT | ARCHIVES | TEACHERS | LINKS | CONTACT
All content on this site is © Massachusetts
Society for Medical Research or others. Please read our copyright
statement — it is important.
|
|
|
|

