Highlights
The nose is the only organ in our body that is constantly exposed to the external environment. These researchers hypothesized that immune mechanisms in the nose might help prevent airborne infections. The investigators exposed nasal cells to bacterial and viral pathogens and characterized the underlying immune response. They showed that the immune response against viral pathogens is decreased at lower temperatures. These results offer a biological explanation for why viral illnesses are more common in colder months. Ongoing research will continue to deepen our understanding of immune mechanisms in the nose. These researchers hope these findings will lead to new remedies for the treatment and prevention of viral illnesses.
Have you ever wondered why we tend to get sicker in cold weather? New research by Dr. Mansoor Amiji at Northeastern University and Dr. Benjamin Bleier at Harvard Medical School shows that lower temperatures make our immune system less effective against viral illnesses. These researchers hope that their findings will provide the foundation for future research into the mechanisms of the immune system in the nose, as well as offer new pathways for treatments to prevent and manage viral illnesses.
The Nose and the Immune System
The nose is unique among organs in our body because it is the only place that is constantly exposed to the outside world. It is the beginning of the respiratory system, a network of organs and tissues that help us breathe, talk, and smell.
We breathe in about 10,000 liters (over 2,500 gallons) of air each day. The air enters through the nose and mouth, travels through the nasal passages and down the
pharynx
to the
trachea.
The trachea, or windpipe, connects the throat to the two large
bronchi
that branch off to each lung. The pathway from the nose to the lungs is known as the
respiratory tract.
The respiratory tract is sometimes divided into the upper respiratory tract (nose, mouth, and pharynx) and lower respiratory tract (trachea, bronchi, and lungs).
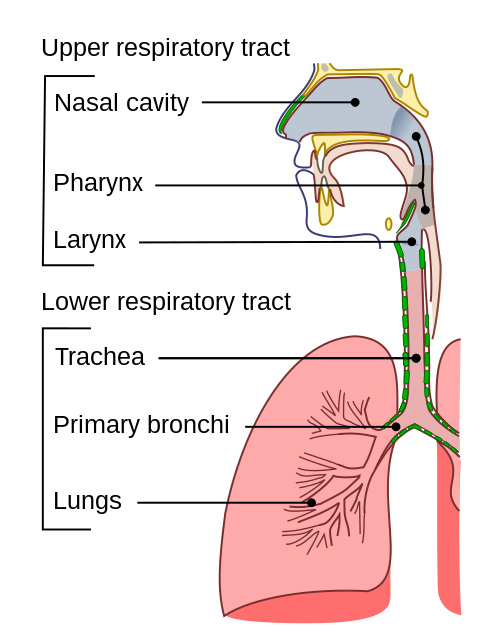
Figure 1. Upper and lower respiratory tract.
[Source: https://en.wikipedia.org/wiki/Respiratory_tract]
The entire respiratory tract is lined with
epithelium,
a thin layer of cells that line organs and glands. Cells of the epithelium are called epithelial cells, and they tend to produce mucus and other substances. Epithelial cells in the nose are called nasal epithelial cells.
The air we breathe brings in the oxygen that we need to survive, but it also exposes us to numerous
pathogens,
such as
bacteria
and
viruses,
that can make us sick. Nasal epithelial cells produce mucus and contain tiny hair-like projections called
cilia,
which act as a physical barrier by filtering dust and other pathogens. These cells also work as part of the immune system to prevent infection.
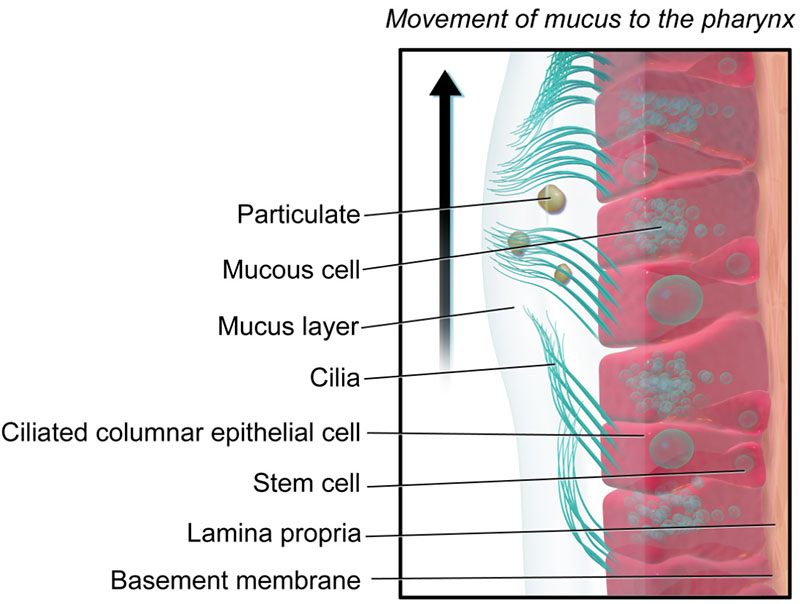
Figure 2. Nasal epithelial cells and cilia.
[Source: https://en.wikipedia.org/wiki/Respiratory_epithelium]
In order to get sick, two things need to happen. First, the body needs to be exposed to the pathogen by inhaling it through the nose or mouth. Second, enough of the pathogen needs to make it through the defense systems in the nose so it can infect cells and cause symptoms. Healthy people are exposed to many more pathogens than the ones that actually make us sick. This is because infection can be prevented if the pathogen can be neutralized by the immune system before even leaving the nose.
The most common types of airborne infections are viruses. Especially in the colder months, viruses can cause illnesses ranging from the common cold to more serious diseases such as
SARS-Cov-2
(the virus that causes COVID-19),
influenza
(the flu), and
respiratory syncytial virus
(RSV).
There is no cure for most infections caused by viruses, only treatments to prevent illness, such as vaccines against influenza and COVID-19, and to reduce symptoms once an infection has developed. Improved understanding of our body’s own immune responses in the nose to prevent and fight infections could lay the foundation for the development of better treatments for viral illnesses.
Experimenting with Nasal Cells
Dr. Benjamin Bleier is an
otolaryngologist,
commonly known as an ear, nose, and throat (ENT) doctor, specializing in problems of these organs. He was interested in understanding how the nose protects itself from infections given that it is constantly exposed to the external environment. To better understand these mechanisms, Dr. Bleier teamed up with Dr. Mansoor Amiji at Northeastern University. Dr. Amiji is a pharmaceutical scientist who studies
drug delivery systems
targeted to specific parts of the body. Dr. Bleier and Dr. Amiji had previously collaborated on multiple projects. Together, they decided to investigate the immune system in the nose.
Scientists had already identified some immune mechanisms in the nose. For example, a family of proteins called toll-like receptor proteins or TLRs are present on the surface of nasal epithelial cells. One function of TLRs is to secrete tiny bubbles known as extracellular vesicles (EVs) that can carry information beyond the cell. There are many kinds of TLRs that are stimulated by different types of pathogens. For example, TLR3 is stimulated by viruses and TLR4 is stimulated by bacteria. Dr. Bleier and Dr. Amiji built off of these previous discoveries in their research.
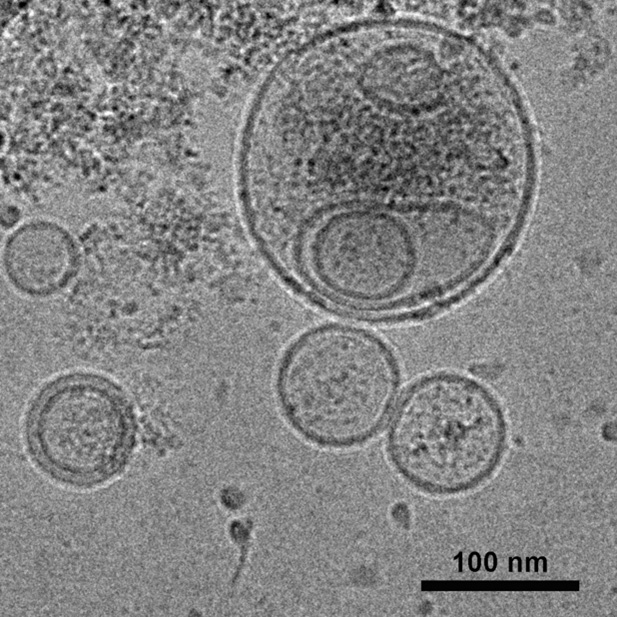
Figure 3. Transmission electron microscopy image of extracellular vesicles derived from human nasal epithelial cells.
[Source: Dr. Di Huang]
To study immunity in the nose, the researchers used nasal epithelial cells taken from healthy volunteers who were undergoing nasal surgery. “There are many reasons why we might perform nasal surgery on a patient,” explained Dr. Bleier. “Sometimes patients have chronic infection or inflammation. We would not take samples from these patients because the presence of the underlying condition might affect our results.” Sometimes patients who are otherwise healthy may undergo nasal surgery for reasons related to the structure of the bones. Patients in these situations were asked if they were willing to offer samples of their nasal cells. Samples were collected from these healthy volunteers using a nasal swab in the operating room. Nasal epithelial cells were isolated from the nasal swab and
cultured
in petri dishes in the laboratory.

Figure 4. Nasal epithelial cells cultured in a 6-well plate.
[Source: Alyssa Stone, Northeastern University]
In initial experiments, Dr. Bleier and Dr. Amiji used cultured nasal epithelial cells to simulate what would happen if bacteria were to enter the nose. They exposed human nasal epithelial cells to surface proteins found on the bacterium Pseudomonas aeruginosa, a common bacterial pathogen. The results showed that the bacterial surface proteins stimulated TLR4 to release twice as many EVs compared to the control condition. Analysis of the EVs showed they contained dozens of immune molecules including those specific to P. aeruginosa.
In a follow-up study, Dr. Bleier and Dr. Amiji performed similar experiments to understand how nasal epithelial cells respond in the presence of viral illnesses. The experiments for this part of the study were conducted by Dr. Di Huang, a postdoctoral research fellow working with Dr. Amiji and Dr. Bleier.
Dr. Huang exposed human nasal epithelial cells to three common types of respiratory viruses. As in the previous experiments, the results showed that all three viruses stimulated TLR3 to release twice as many EVs compared with controls. The contents of the EVs included immune molecules specific to fighting viral infections. In addition, TLR3 released
surface receptor
proteins that act as a decoy for the virus, meaning that the virus would bind to the decoys and be destroyed rather than binding to cells they could infect.
Taken together, these results showed that human nasal epithelial cells have a three-pronged response to neutralize viral infections:
- Two-fold increase in release of EVs
- EVs contain immune molecules targeted to the pathogen
- Release of surface receptor proteins as viral decoys
Temperature and the Immune Response
Next, the researchers investigated whether the immune response of the nasal epithelial cells was affected by temperature. “We know that viral illnesses increase during the colder months,” explained Dr. Amiji. “We wondered whether this might be due to weakened immunity in the nose.”
To find out, the researchers first needed to know how changes in environmental temperature affected the nose. They asked healthy volunteers to brave the cold as room temperature dropped from 73.4°F to 39.2°F. At 73.4°F, the temperature inside the nose of volunteers was 98.6°F, normal body temperature. At 39.2°F, the temperature inside the nose dropped to 89.6°F, a difference of 9°F.
Dr. Huang used this information to expose cultured nasal epithelial cells to a drop of 9°F. The results showed a decrease in EVs, decrease in EV contents, and decrease in surface receptor proteins. “This is a pretty remarkable result,” explained Dr. Amiji. “All three prongs of the immune system’s multipronged approach to prevention of viral illness were decreased.”
Protect Yourself against Viral Infection
Based on these results, the researchers believe they have found an underlying biological mechanism for why we get sicker in the cold: colder temperatures lead to a decrease in immune protection in the nose.
“Even though our nose has less immune protection in the cold, there are still ways to protect yourself against winter illness,” commented Dr. Bleier. You are probably familiar with precautions against viral illnesses, since it is the same advice given to protect yourself against infection by SARS-Cov-2, the virus that causes COVID-19: wash your hands frequently, avoid touching your face with unwashed hands, and frequently disinfect commonly touched surfaces.
Figure 5. How to stop the spread of germs, from the Centers for Disease Control and Prevention.
[Source: https://www.maine.edu/together/wp-content/uploads/sites/72/2020/03/CDC-Poster-Accessible.UMS_.Logo_.3.4.20-1.pdf]
Another way to protect against viral illnesses that we know well: wear a mask. “We have not yet shown this scientifically, “added Dr. Bleier, “but this could also be a reason why masks are so effective at preventing infection by SARS-Cov-2. Since masks provide an extra barrier between the nose and the environment, they might help maintain the temperature, and therefore the immune protection, in the nose.”
Dr. Amiji and Dr. Bleier have many ideas for future research. They would like to further analyze the EVs to better understand what they contain and how they function. They also want to know more about how the surface receptor proteins work as viral decoys and how the nasal epithelial cells are able to communicate to each other about incoming threats. Ultimately, the researchers hope their findings will lead to future treatments for viral illnesses and more ways to prevent such infections.
In addition, these findings have the potential to open new avenues for research into the lungs. This is because of a new model called the unified airway that suggests that the lining of the entire respiratory tract, from the nose to the lungs, is similar. It is very difficult to conduct experiments on lung tissue in the way that Dr. Amiji, Dr. Bleier, Dr. Huang, and colleagues have done for nose tissue, because lung tissue is not easily accessible. “Under the unified airway model, our research to better understand immune mechanisms in the nose also increases our understanding of the lungs and possibly diseases of the lungs,” concluded Dr. Bleier.
Dr. Mansoor Amiji is a University Distinguished Professor in the Departments of Pharmaceutical Sciences and Chemical Engineering at Northeastern University. His research focuses on drug delivery systems such as medications and vaccines for a variety of medical problems. When not in the laboratory, Dr. Amiji enjoys spending time with his family, traveling both within the United States and abroad, and participating in sports activities.
Dr. Benjamin Bleier is Associate Professor of Otolaryngology at Harvard Medical School and Chair of Otolaryngology–Head and Neck Surgery at the Massachusetts Eye and Ear Institute. He is a researcher-clinician who both sees patients and is involved in multiple research projects. When not in the laboratory, Dr. Bleier enjoys playing tennis and spending time with his family.
Dr. Di Huang is a postdoctoral research fellow at Northeastern University and Massachusetts Eye and Ear Institute, where she works closely with Dr. Amiji and Dr. Bleier. When not in the laboratory, Dr. Huang enjoys cooking, traveling, and spending time outdoors.
For More Information:
- Huang, D. et al. 2022. “Cold exposure impairs extracellular vesicle swarm–mediated nasal antiviral immunity.” Journal of Allergy and Clinical Immunology. https://www.jacionline.org/article/S0091-6749(22)01423-3/fulltext
- Nocera, A. et al. 2018. “Exosome swarms eliminate airway pathogens and provide passive epithelial immunoprotection through nitric oxide.” Journal of Allergy and Clinical Immunology. https://www.jacionline.org/article/S0091-6749(18)31351-4/fulltext
To Learn More:
- Amiji Lab. https://web.northeastern.edu/amijilab/
- Bleier Lab. https://projects.iq.harvard.edu/bleierlab
- Jaslow, R. “Why Upper Respiratory Infections Are More Common in Colder Temperatures.” Mass Eye and Ear Communications, 5 Dec 2022. https://hms.harvard.edu/news/why-upper-respiratory-infections-are-more-common-colder-temperatures
- ENT Health. https://www.enthealth.org/
Written by Rebecca Kranz with Andrea Gwosdow, PhD at www.gwosdow.com
HOME | ABOUT | ARCHIVES | TEACHERS | LINKS | CONTACT
All content on this site is © Massachusetts
Society for Medical Research or others. Please read our copyright
statement — it is important. |

