Highlights
Lyme disease is a tick-born infection that can cause chronic illness in some patients even after treatment with antibiotics.
These researchers searched for an antibiotic that would be selectively effective against the bacteria that causes Lyme disease. They rediscovered the antibiotic Hygromycin A that effectively treated Lyme disease in mice.
These researchers have partnered with a pharmaceutical company to continue to study Hygromycin A and develop it into an antibiotic that could be used to treat patients with Lyme disease. They continue to search for new antibiotics to treat the bacteria that causes Lyme disease and other chronic infections.
Did you know that most
antibiotics you might be prescribed by the doctor were invented by bacteria in the soil? The soil is filled with millions of bacteria that must fight each other to survive. One of the tools bacteria use to beat their opponents is compounds to weaken and kill other bacteria around them. By isolating these compounds from the bacteria that produce them, researchers make these defense mechanisms available to humans when bacteria have infected our bodies. For example, the first successful antibiotic, penicillin, is produced by the soil bacteria, Penicillium.
Antibiotics are critical medications that help us fight diseases caused by bacterial infections. “Science went through a golden age of antibiotic discovery in the 1940’s and 1950’s,” explained Dr. Kim Lewis, Distinguished Professor of Biology at Northeastern University. Since that time, the use of antibiotics has become widespread, and many common bacterial infections have become resistant to the antibiotics we have available. “We critically need to identify novel antibiotics that could treat a wide variety of illnesses,” added Dr. Nadja Leimer, Postdoctoral Research Associate in Dr. Lewis’s lab. This is the goal of the Antimicrobial Discovery Center directed by Dr. Lewis.
It is important to note that not all antibiotics are alike. Some antibiotics, known as
broad spectrum antibiotics,
can treat a wide range of bacterial infections. Other antibiotics are more selective for specific types of bacteria. The advantage of broad-spectrum antibiotics is that they can be used before doctors have identified the specific bacteria causing an infection. However, since broad-spectrum antibiotics can kill a wide range of bacteria, they generally wipe out all the bacteria in our gut, both good and bad. This can cause digestive issues, among other symptoms, in patients taking antibiotics.
Lyme Disease
One bacterial infection that the Lewis Lab has been working on for some time is
Lyme disease.
Lyme disease is an infection caused by the bacteria Borreliella burgdorferi that is transferred from rodents to humans via the deer tick Ixodes scapularis.
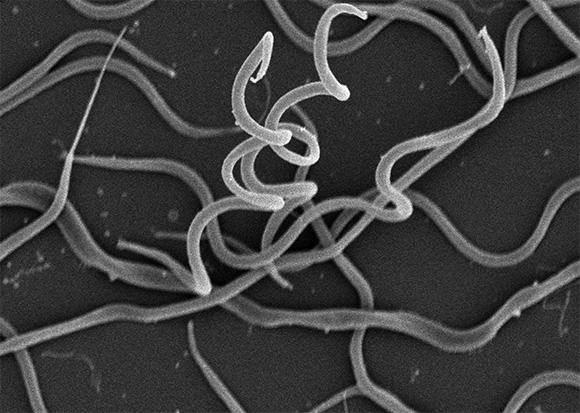
Figure 1. Spiral-shaped Borreliella spirochete bacteria
[Source: Dr. Lewis and Dr. Leimer]
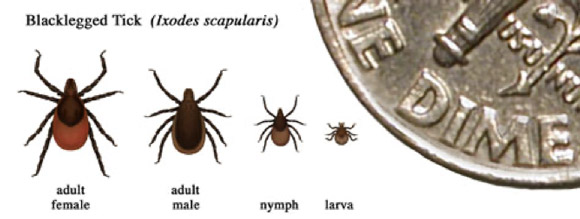
Figure 2. Ixodes scapularis also known as deer tick. Here seen with a dime for reference
[Source: https://www.cdc.gov/lyme/transmission/blacklegged.html]
Most people who develop Lyme disease after a tick bite will notice a target-shaped rash around the bite site.

Figure 3. Classic target-shaped rash from a tick infected with Borreliella burgdorferi, the bacteria that causes Lyme disease
[Source: https://www.cdc.gov/lyme/signs_symptoms/rashes.html]
These patients are prescribed a broad-spectrum antibiotic for two weeks, which typically clears the infection. However, in about 10% of patients, the disease progresses into a chronic condition known as
post-treatment Lyme disease syndrome (PTLDS),
characterized by persistent pain, fatigue, and decreased cognitive function. Little is known about PTLDS and how to treat it.
As a researcher focused on antibiotic discovery, Dr. Lewis noticed that patients with PTLDS already had digestive problems and imbalance of gut bacteria. He wondered if these patients could be helped by a more selective antibiotic that would only target B. burgdorferi and not the good bacteria of the gut. “An antibiotic that was selective against B. burgdorferi had never been identified,” recalled Dr. Lewis. “As an antibiotic discovery laboratory, we wanted to take on this challenge.”
Searching for Selective Antibiotics
Dr. Lewis and his team turned to soil bacteria for answers. Their goal was to find a compound that selectively killed B. burgdorferi but would not affect other types of bacteria. To do this, they tested hundreds of known soil bacteria for their effects against two infection-causing bacteria: B. burgdorferi and Staphylococcus aureus. “If a compound killed both B. burgdorferi and S. aureus, we weren’t interested,” described Dr. Lewis. Such a compound would result in a broad-spectrum antibiotic, and the researchers were looking for an antibiotic that would be selective only for B. burgdorferi.
The researchers identified one type of bacteria, Streptomyces hygroscopicus, that produced an antibiotic selective only for B. burgdorferi. When they isolated the antibiotic compound in the bacteria, they realized it was a known antibiotic first discovered in 1953, known as Hygromycin A. Hygromycin A was not an effective antibiotic like many of the others commonly used today, so the team that discovered it did not do follow-up studies. Upon rediscovering Hygromycin A, Dr. Lewis and his team found that, while it may not be an effective broad-spectrum antibiotic, it was very effective against B. burgdorferi.
Once the researchers identified Hygromycin A as a potential compound selective against B. burgdorferi, they conducted follow-up experiments to determine its safety and effectiveness in mice.
Figure 4. Dr. Leimer (left) and Dr. Lewis (right) conducting studies in the laboratory
[Source: Dr. Leimer and Dr. Lewis]
These studies showed that Hygromycin A was very safe and highly effective at fighting infection in mice with Lyme disease. Importantly, the researchers also determined that Hygromycin A does not impact gut bacteria. “We liked everything we saw about this compound,” reflected Dr. Leimer, “but we still didn’t understand why it worked.”
B. burgdorferi belongs to a class of bacteria called spirochetes,
named for their unique spiral shape. Spirochetes are unlike any other class of bacteria in the world, with distinct physical properties and a completely different genetic structure. In addition to Lyme disease, spirochetes also cause
syphilis,
a common sexually transmitted disease, and periodontal (gum) disease in the mouth.
The researchers studied the structure of B. burgdorferi and its interaction with Hygromycin A to better understand the underlying mechanisms for why the newly rediscovered antibiotic was only selectively effective against spirochetes. They identified a particular transporter protein called BmpDEFG that allows Hygromycin A into the bacteria. This transporter is found only in spirochete bacteria, which is what makes Hygromycin A so effective at selectively killing them.
Drs. Lewis and Leimer and colleagues identified Hygromycin A as an effective treatment for Lyme disease in mice. The next step is to conduct further testing in larger animals. In addition, the treatment needs to be made into a pill that could be used in future clinical trials with humans. “That is outside the scope of what we do in the laboratory,” explained Dr. Lewis, “so we have partnered with a company called FlightPath that will conduct the testing needed to determine whether Hygromycin A could be an effective treatment for Lyme disease in humans.” In addition, further studies will determine whether Hygromycin A might be an effective treatment for other diseases caused by spirochetes such as syphilis and periodontal disease.
Eradicating Lyme Disease Transmission in the Wild
Treatment for people with acute Lyme disease and PTLDS is critically important. In addition, Lyme researchers continue to study the possibility of eradicating Lyme disease in the wild. Lyme disease in humans is caused by the bite of an infected tick, but the tick got the disease from another infected animal.
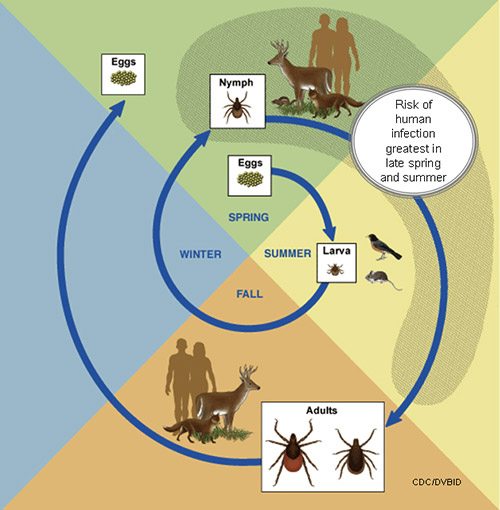
Figure 5. The life cycle of the deer tick that transmits Lyme disease. The most common route of transmission is from mice to deer to humans
[Source: https://www.cdc.gov/lyme/transmission/blacklegged.html]
The animal most responsible for Lyme transmission in the wild is mice. If, as Drs. Lewis and Leimer have shown in the laboratory, Hygromycin A effectively defeats the B. burgdorferi infection in mice, it is possible to imagine curing the infection of B. burgdorferi -carrying mice in the wild. Drs. Lewis and Leimer are hopeful that Hygromycin A or another antibiotic found to be selective for spirochetes may eradicate the transmission of Lyme disease in the wild.
Drs. Lewis and Leimer hope to find multiple antibiotics that are selective for B. burgdorferi. Their next steps continue to focus on identifying additional antibiotics with similar effectiveness to Hygromycin A. “Right now, Hygromycin A looks really promising in our mouse studies,” commented Dr. Lewis, “but you never know what might happen.” This is why the researchers are looking for multiple possible treatments.
Dr. Kim Lewis is a Distinguished Professor of Biology and Director of the Antimicrobial Discovery Center at Northeastern University. He has dedicated his career to the discovery of novel antibiotics and research into chronic infectious diseases such as chronic Lyme disease. When not in the laboratory, Dr. Lewis enjoys reading fiction and kayaking.
Dr. Nadja Leimer is a Postdoctoral Research Fellow in the laboratory of Dr. Kim Lewis at Northeastern University. Her research interests include the mechanisms by which bacteria evade antibiotics. When not in the laboratory, Dr. Leimer enjoys hiking and running.
To Learn More:
- Leimer, N. et al. “A selective antibiotic for Lyme disease.” Cell, 184(21): P5405-18. https://www.cell.com/cell/fulltext/S0092-8674(21)01058-8
- 1. Le Page, M. Drug treatment for lyme disease could lead to its eradication. New Scientist, October 6, 2021. https://www.newscientist.com/article/2292543-drug-treatment-for-lyme-disease-could-lead-to-its-eradication/?utm_medium=social&utm_campaign=echobox&utm_source=Facebook&fbclid=IwAR3XCBZ6-RJWPkb9kke8UcmWDe-4m
For More Information:
- Lewis Lab. https://web.northeastern.edu/adc/
- Centers for Disease Control and Prevention. https://www.cdc.gov/lyme/index.html
- National Institute of Allergy and Infectious Disease. https://www.niaid.nih.gov/diseases-conditions/lyme-disease
- Massachusetts Department of Public Health. https://www.mass.gov/service-details/lyme-disease
- American College of Rheumatology. https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Lyme-Disease
Written by Rebecca Kranz with Andrea Gwosdow, PhD at www.gwosdow.com
HOME | ABOUT | ARCHIVES | TEACHERS | LINKS | CONTACT
All content on this site is © Massachusetts
Society for Medical Research or others. Please read our copyright
statement — it is important. |

