| |
Did you know that you are actually slightly taller in the morning than at night?
That’s because over the course of the day the weight of your head, neck, and shoulders compress the space between the
vertebrae
in your
spinal cord.
Then, while you sleep, your spine has a chance to lengthen and take back some of the space lost during the day. So when you wake up, you’re just a tiny bit taller than when you went to sleep.
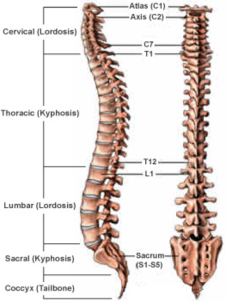
Humans are born with 33 separate vertebrae.
By adulthood, we typically have 24 due to the fusion of the vertebrae in the sacrum. The top 7 vertebrae that form the neck are called the cervical spine. The upper back, or thoracic spine, has 12 vertebrae. The lower back, or lumbar spine, has 5 vertebrae. The sacrum (S1) and coccyx (tailbone) are made up of 9 vertebrae that are fused together to form a solid, bony unit.
http://www.neurospineinstitute.org/spinal-procedures/spine-anatomy-and-physiology
The spine is made up of 33 individual bones called vertebrae that extend from your tailbone to your neck. The vertebrae provide structure and allow for movement and flexibility in the back. They also protect the spinal cord, which contains bunches of nerve fibers and other cells that transmit messages from the brain to the rest of the body and back. The vertebrae are connected together in the back by numerous muscles and
ligaments
and in the front by specialized organs called
intervertebral discs.
An intervertebral disc
http://www.spineuniverse.com/anatomy/intervertebral-discs
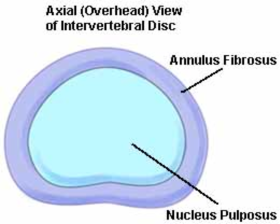
Intervertebral discs are like filled-in tires. They contain a jellylike center, called the
nucleus pulposus,
and a tougher outer layer which is surrounded by the tougher
annulus fibrosus.
Together the intervertebral discs absorb the shock of daily activity and act like miniature joints in the way they allow for movement between the vertebrae.
Over many decades of routine activity, intervertebral discs can start to degenerate. This is a leading cause of neck and back pain. In many people, treatments to alleviate pain and reduce inflammation include anti-inflammatory drugs, pain medications, and physical therapy to strengthen back and core muscles.
This Really Hurts
When you get a tear in the annulus fibrosus, it results in a
herniated disc.
A tear, resulting from disc degeneration will often heal itself over the course of
weeks or months.
For some patients, though, a herniated disc can cause part of the nucleus pulposus to extrude out of the disc and push against the nerves of the spinal cord.
In patients who have failed all non-operative treatments, the best way to relieve this type of pain is through surgery.
In milder cases, the operation for a herniated disc will just involve the removal of the protruding nucleus.
If there is significant injury, however, it may be necessary to remove the entire disc. For many decades, when a disc was removed the vertebrae above and below the removed disc were then joined (fused) together. This is not a great solution, however, because the rest of the spine has to compensate for the lost disc, which can result in degeneration and the development of arthritis in other parts of the back. In the past five years, metal and plastic implants have been developed to replace the removed disc. These implants allow for more flexibility in the spine, but they are still not an ideal solution because they can pop out, fracture, or wear away over time.
Better Implants
Five years ago, Dr. Lawrence Bonassar, a biomedical and mechanical engineer, and Dr. Roger Härtl, a neurosurgeon, both associated with the Weill Cornell Medical Center in New York, teamed up to find a biological alternative to artificial spinal disc implants. When they began working together, Dr. Bonassar and his team of researchers had already developed a prototype for bioengineered disc implants. They grow the nucleus pulposus and the annulus fibrosus separately from different types of sheep cells.
The researchers use
collagen,
a fibrous connective tissue, as a base for creating the annulus fibrosus. The disc is created with a hole in the center, and the nucleus pulposus is then inserted to fill the hole. There were many different ways to create the implants by varying the types of material, the number of cells used, and the density of the cells. After many years of laboratory research, Dr. Bonassar wanted to see how his different spinal disc models performed in a living organism. That’s where Dr. Härtl comes in.
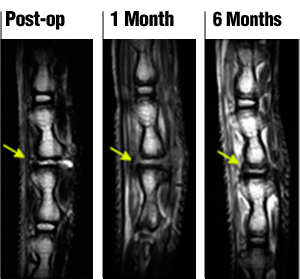
Follow up MRI after implanting the discs in a rat tail between the 3rd and 4th vertebra of the rat tail spine
Dr. Härtl was familiar with animal models and suggested testing the discs in rat tails, which have vertebrae that could readily be removed and replaced. The discs were implanted into the tails of rats for about six months. Then the researchers took images of the discs with
Magnetic Resonance Imaging,
and X-rays and performed some tests of biomechanical function of the discs. The tests were designed to show whether the bioengineered disc acted like a normal disc. After each round of experiments, Dr. Bonassar and his team would go back to work improving upon their bioengineered implant based on the results of Dr. Härtl’s experiments.
Through these experiments, Drs. Bonassar and Härtl created an artificial disc that can replace intervertebral discs. This intervertebral disc, when implanted into rats, acts like a “real” disc that can withstand the pressure and movement of the spine. With time, this artificial intervertebral disc integrates into the spine and cannot be distinguished from natural discs.
"This is still a very basic model," Dr. Härtl commented. "But the results are promising."
Moving Towards Humans
The next step for their research is to replicate these experiments in larger animals such as sheep or goats. This would require Dr. Bonassar and his team to grow larger discs, a process that has already begun. If these researchers can achieve the same results in these larger animals as they did in rats, the next step would be a human model. "But that’s at least five or ten years away," cautioned Dr. Härtl.

TE-Disc (synthetic) compared to the native disc and 6. months after explanting the Te-Disc
Dr. Roger Härtl is Associate Professor of Neurological Surgery and Chief of Spinal Surgery and Neurotrauma at Weill Cornell Medical College in New York. His research interests focus on the development of bioengineered spinal disc for use in surgical operations on humans. Dr. Härtl is also the neurosurgeon for the New York Giants football team, which requires him to attend all Giants football games! In addition, Dr. Härtl trains neurosurgeons in Africa through the Global Health Initiative at Cornell Medical College. When not in the lab, operating room, or football game, Dr. Härtl also enjoys skiing and mountaineering. Dr. Härtl’s collaborator, Dr. Larry Bonassar, is Associate Professor of Biomedical Engineering and Mechanical and Aerospace Engineering at Cornell University.
For More Information:
- Bowles, R. et al. 2011. "Tissue-engineered intervertebral discs produce new matrix, maintain disc height, and restore biomechanical function to the rodent spine." Proceedings of the National Academy of Sciences, 108(32): 13106-13111.
- Bowles, R. et al. 2010. "Self-Assembly of Aligned Tissue-Engineered Annulus Fibrosus and Intervertebral Disc Composite Via Collagen Gel Contraction." Tissue Engineering, 16(4): 1339-1348.
To Learn More:
- American Association of Neurological Surgeons.
http://www.aans.org/Patient%20Information/Conditions%
20and%20Treatments/Herniated%20Disc.aspx
- Ohio State University Medical Center.
http://medicalcenter.osu.edu/patientcare/healthcare_services/
nervous_system/disc/Pages/index.aspx
Rebecca Kranz with Andrea Gwosdow, PhD www.gwosdow.com
HOME | ABOUT | ARCHIVES | TEACHERS | LINKS | CONTACT
All content on this site is © Massachusetts
Society for Medical Research or others. Please read our copyright
statement — it is important. |
|
|
 Dr. Roger Härtl

Dr. Lawrence Bonassar

Dr. Härtl explains the benefits of organic discs vs. the others currently available. There is also footage of his surgical team at work.
Back Injury is Nothing New
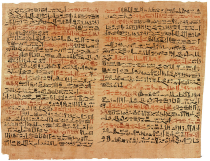
The Edwin Smith Papyrus (above), a medical text from ancient Egypt (c. 1600 BCE) includes instructions for dealing with various medical conditions and injuries, including back problems. It is based on a medical text from 1,000 years earlier, perhaps for physicians who treated workers hurt while constructing the pyramids. The final section of the papyrus, treatment of vertebral injuries, is unfortunately incomplete, so we don’t know what the physician was supposed to do after his diagnosis.
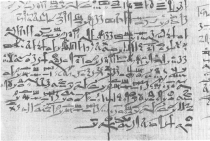
The final section of the Edwin Smith Papyrus. This part of the papyrus, treatment of vertebral injuries, is incomplete, so we don’t know what the physician was supposed to do after his diagnosis.
DIAGNOSIS
Thou shouldst say concerning him: "One having a sprain in a vertebra of his spinal column. An ailment which I will treat."
TREATMENT
Thou shouldst place him prostrate on his back; thou shouldst make for him ...
Sign Up for our Monthly Announcement!
...or  subscribe to all of our stories! subscribe to all of our stories!

What A Year! is a project of the Massachusetts
Society for Medical Research.
|
|

