|
What do peanut allergies and the degenerative disease multiple sclerosis have in common? The immune system! Or, improper immune response, to be more precise.
The
immune system
is composed of organs and specialized cells that work together to fight infection and disease. In order to do this, the immune system must distinguish between substances that keep us healthy and those that could pose a threat to our well-being. As immune cells develop, they recognize potentially harmful invaders like bacteria and viruses and distinguish them from the thousands of other compounds we need to survive. When the immune system identifies a foreign agent, certain immune cells either destroy it or begin producing proteins called
antibodies
that bind specifically to the unwanted agents and destroy them, thereby preventing infection. Anything that produces an immune response is known as an
antigen.
In healthy people, the immune system can correctly target potentially harmful antigens and ignore all the other cells and organisms that actually belong in the body. The ability to recognize parts of the body that belong is called
tolerance.
The immune system is said to be tolerant of the self and non-threatening substances when they do not produce immune responses.
But sometimes the immune system may not develop tolerance
towards benign compounds or it may lose tolerance later in life.
This can result in a variety of disorders from mild allergies to debilitating illnesses and even death. In the case of allergies, the immune system mistakenly identifies a particular non-harmful substance, such as
peanuts,
shellfish or pollen, as an antigen and launches an immune response. This allergic reaction is the immune system responding to these allergens as it would an infection.
In the case of
autoimmune disease
the immune system loses its tolerance to particular tissues and mistakenly targets healthy cells as antigens. There are over 80 known autoimmune disorders including
rheumatoid arthritis,
lupus,
type 1 diabetes
and
multiple sclerosis.
Weakening the Immune System
The only treatments available for autoimmune disorders are a class of drugs aptly named immunosuppressants because they suppress the entire immune system. This weakens the immune response against the antigen causing the autoimmune disease, but it also weakens the rest of the immune system just as much—it leaves the patient vulnerable to all kinds of infections and to an increased chance of developing cancer. As a result, while immunosuppressants may reduce the symptoms of disease, they can also severely decrease the quality of life for patients. Still, immunosuppressants are the best available option to treat many diseases and provide needed relief for patients.
A better alternative to the systemic treatment of autoimmune diseases with immunosuppressants would be specific therapies that target only the particular antigen(s) involved. This approach is known as antigen-specific therapy.
Dr. Stephen Miller of Northwestern University has dedicated much of his career to the development of antigen-specific therapy to treat the autoimmune disease multiple sclerosis. Multiple sclerosis, or MS for short, is the result of an immune attack against the
myelin sheath
that protects nerve cells of the brain and spinal cord. The symptoms and severity of the disease vary widely based on the frequency of attacks and where in the brain they occur. There is no cure for multiple sclerosis, and treatment focuses on relieving symptoms and slowing the progression of disease. The most common treatments for multiple sclerosis are immunosuppressant drugs.
The underlying problem in patients with MS is that, for some reason, their immune systems lose tolerance for myelin molecules and try to destroy them. "If we were able to once again make the immune system tolerant towards myelin," Dr. Miller explains, "in theory we would be able to stop the disease in its tracks."
Work in Mouse Models
This is exactly what Dr. Miller has done in mouse models of multiple sclerosis. His method of antigen-specific therapy tricks the immune system into thinking that the myelin proteins are normal, thus inactivating the immune response that was causing the disease. To do this, he first takes a blood sample from the mice and gathers all the white blood cells, which are responsible for the immune response. He then chemically attaches myelin proteins onto the surface of these white blood cells and reinfuses them back into the patient. In so doing, Dr. Miller induces tolerance towards the myelin proteins that are normally present in healthy patients.
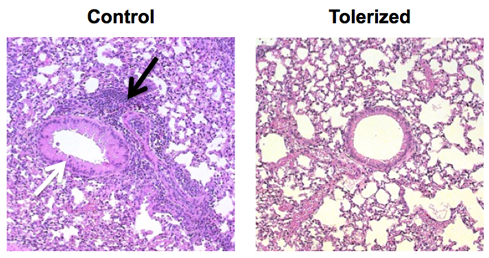
Tolerance Prevents Airway Thickening and Inflammation in a Model of Allergic Airway Disease
Left panel shows that introduction of ovalbumin (egg protein) to the lungs of a mouse with allergy to egg protein leads to thickening of the airway (white arrow) and the influx of a massive number of inflammatory leukocytes (black arrow). This response is prevented in mice which were tolerized to the ovalbumin protein prior to lung challenge—this lung looks the same as it does in a normal mouse.
This treatment was so successful in mice that tests on human patients, known as clinical trials, began several years ago. The first phase of these clinical trials has now been completed, and the treatment has been established as safe for human use.
Dr. Miller developed this antigen-specific therapy for the treatment of multiple sclerosis, but he hypothesized that the same method could be used to treat a variety of other conditions caused by an adverse immune response. One evening he was chatting with his colleague Dr. Paul Bryce, an allergist at Northwestern University. They decided to try the same method in mice that were allergic to peanuts.
As we discussed earlier, allergies and autoimmune disorders like MS are caused by the same mistaken immune response. In autoimmune disease, the response is against your own tissue; in the case of allergies, the response is against something you might eat or breathe. In patients with severe allergies, antigens may cause
anaphlaxis, also known as anaphylactic shock. This is a systemic reaction to the allergen that mobilizes all the body's immune resources to fight a needless battle against the antigen.
Anaphylaxis is dangerous because it causes the throat to swell and may cause suffocation if not treated immediately.
To test whether this method might work to treat peanut allergies in addition to multiple sclerosis, the researchers removed white blood cells from mice with similar peanut allergies to humans and chemically attached a peanut extract protein to the surface of these white blood cells. This complex of white blood cells and peanut extract was then injected back into the same mice. The mice, that were originally allergic to the peanut extract, did not have any allergic reactions to the re-injected complex of white blood cells and peanut extract. This was in contrast to allergic mice that were exposed to the antigen but not treated, and anaphylaxis ensued as a result.
Through these experiments, Drs. Miller and Bryce demonstrated that they could prevent an allergic reaction in mice that were originally allergic to peanuts by applying this method of antigen-specific therapy. One advantage of this method is that it targets only the cells causing the unwanted immune response and does not affect other cells in the body. Given the success of similar treatment methods in mice with MS and promising results from human trials, these researchers hope their studies will eventually lead to the development of a cure for many types of allergies.
On to Organ Transplants
Dr. Miller is also excited about the possibilities of using antigen-specific therapy to induce tolerance in patients who have received an organ transplant.
When foreign tissue enters the body, as it does during an organ transplant, the immune system responds by attacking the transplanted tissue. In order to reduce the immune response and allow the transplanted organ to function properly, patients who are going to receive transplants must start on immunosuppressant drugs and may have to remain on them for the rest of their lives. If antigen-specific therapy could be used to induce tolerance towards the foreign tissue, it would enable recipients of organ transplants to lead fuller, healthier lives.
In initial experiments with organ transplantation in mice, Dr. Miller has shown his method to be equally effective as in multiple sclerosis and peanut allergy. He has performed experiments by taking
pancreatic islet cells
from one mouse and transplanting them into a second mouse which has diabetes. With no intervention, the recipient mouse rejects the donated islet cells within two weeks. If the recipient mice were treated with white blood cells from an
apoptotic donor, however, they were able to survive up to a year without any rejection. Dr. Miller is currently collaborating with researchers at the University of Minnesota to test this method in non-human primates (rhesus monkeys) that are more similar to humans than mice. If those studies are successful, the next step would be human trials.
From White Cells to Particles
Dr. Miller is extremely enthusiastic about the results this method has shown so far. He is starting a company to develop antigen-specific treatments for human use. One of the largest barriers to the large-scale success of this tolerance-inducing procedure is the time, energy, and money needed to remove white blood cells from blood. Rather than using human blood cells as the attachment molecule for the antigen, he is looking to use synthetic particles that could be created in the laboratory. A manufacturer can produce a biodegradable substance to be formed into spheres about the same size as cells. "Commercially available treatment is still years away," cautions Dr. Miller. "But we want to see this help people as soon as possible."
To date, he and his team have tried their technique in models of multiple sclerosis, type 1 diabetes, peanut allergies, and organ transplants, but there are many more autoimmune diseases that could some day be treated in a similar way.
Dr. Stephen Miller is a Professor of Immunology and Director of the Interdepartmental
Immunology
Center at Northwestern University. His research focuses on the development of antigen-specific therapy for allergies and autoimmune diseases. When not in the lab, Dr. Miller enjoys being outdoors and spending time with his family.
For More Information:
- Smarr, C. et al. 2011. "Antigen-Fixed Leuocytes Tolerize Th2 Responses in Mouse Models of Allergy." Journal of Immunology, 187: 5090-5098.
- Turley, D. and S. Miller. 2010. "Prospects for Antigen-Specific Tolerance Based Therapies for the Treatment of Multiple Sclerosis." Results and Problems in Cell Differentiation, 51: 217-235.
- Miller, S. et al. 2007. "Antigen-specific tolerance strategies for the prevention and treatment of autoimmune disease." Nature Reviews Immunology, 7:665-675.
To Learn More:
Rebecca Kranz with Andrea Gwosdow, PhD Gwosdow Associates
HOME | ABOUT | ARCHIVES | TEACHERS | LINKS | CONTACT
All content on this site is © Massachusetts
Society for Medical Research or others. Please read our copyright
statement — it is important. |

